Asian Review for Public Administration (ARPA)
Open Access | Research Article | First published online December 20, 2023
Vol. 31, Nos. 1&2 (January 2020 to December 2023)
Surviving the Crisis: Making Intergovernmental Relations Strong for Fighting the Pandemic, Case from Nepal
Trilochan Pokharel
Trilochan Pokharel
"Cite article"Pokharel, T. (2020-2023). Surviving the Crisis: Making Intergovernmental Relations Strong for Fighting the Pandemic, Case from Nepal. Asian Review for Public Administration, Vol. 31, Nos. 1&2, 23-46. |
| ||
Abstract: The aftermath of the COVID-19 pandemic is still scary for many countries. Despite having a relatively lower number of casualties compared to some advanced countries, the developing and transitional countries witnessed social and economic impacts. Nepal, an emerging economy, has been accelerating to institutionalize the recent constitutional and political transformation implemented through the 2015 Constitution. The recently adopted federal form of governance has shared state authorities among the federal, provincial, and local governments including management of health services and other emergencies. This new set of governance arrangements has been expected to deliver public services and protect people’s fundamental rights in an efficient, coordinated, and economic way. For a disaster-prone country like Nepal, the COVID-19 crisis exposed its weary and transitional crisis governance. Several gaps have been identified in the ways the government took initiatives. The major challenges were about the defined leadership roles, intergovernmental coordination, indicator-based financial allocation, and capacity of crisis management institutions, including the health care facilities. This paper analyzes Nepal's efforts to manage COVID-19 in the broader landscape of political governanceand disaster risk profiles and offers insights on intergovernmental relations drawing from three rounds of surveys conducted between 2020 and 2021 among Nepal’s local governments.
The studies record a positive response to the functions of local governments as they felt accountable for addressing public concerns. It further reports a number of critical gaps in intergovernmental relations for dealing with COVID-19. Discrete leadership and poor vertical and horizontal coordination and communication, mismatch in funding and COVID-19 caseload and lack of post-recovery plan at all levels of the government made the crisis governance inefficient, increasing the burden on people. Extensive interactions and engagement, organized and collaborative leadership among the orders of the government and strengthening the capacity of the sub-national governments would be instrumental in dealing with such crises in the future.
The studies record a positive response to the functions of local governments as they felt accountable for addressing public concerns. It further reports a number of critical gaps in intergovernmental relations for dealing with COVID-19. Discrete leadership and poor vertical and horizontal coordination and communication, mismatch in funding and COVID-19 caseload and lack of post-recovery plan at all levels of the government made the crisis governance inefficient, increasing the burden on people. Extensive interactions and engagement, organized and collaborative leadership among the orders of the government and strengthening the capacity of the sub-national governments would be instrumental in dealing with such crises in the future.
1. Introduction and Country Background
Nepal is at the 107th position of 195 countries in the Global Health Security Index 2021, a global comparative index that measures the status of health governance in the aftermath of the COVID-19 pandemic (Bell & Nuzzo, 2021). The index provides estimates on six categories of COVID management - prevention, detection and reporting, rapid response, health system, commitments to improving national capacity, financing, and global norms, and risk environment. Among others, the report further highlights two critical issues for dealing with a health crisis: a) insufficient health capacity and b) ineffective coordination among national entities and global organizations. Nepal’s rank is below the global average, indicating potential gaps in the institutional capacity of managing health crises. Considering the constrained healthcare capacity, this paper aims to explore the functioning of the newly implemented federal governance structure of Nepal following the promulgation of the Constitution of Nepal in 2015, particularly from the perspective of coordination among the orders of the governments.
The COVID-19 pandemic has forced all countries, especially the low- and middle-income countries that have a poor health governance system, to assess their health governance capacities and take necessary steps to be prepared for a better future. For a developing country like Nepal, surviving the crisis is always a social, political, economic, governance, and policy issue. This paper focuses on the aspects of intergovernmental relations for managing the health crisis.
Nepal is practicing three-tier multi-level governance with each level having constitutionally enumerated competencies including the management of health services. As the new governance architecture replaced the unitary form of governance with a devolved federal structure, the transition was accelerating, and Nepal was struggling to institutionalize the constitutional provisions by installing governance structures and procedures (Thapa, Bam, Tiwari, Sinha, & Dahal, 2019). Meanwhile, COVID-19 emerged as a real assessment of the country's capacity to deal with the crisis. Considering that public health is a shared responsibility among the levels of government, the theory of intergovernmental relations underscores effective interactions among the governing units are vital in delivering services efficiently. Such interactions should be defined by processes and institutions (Phillimore, 2013) that would facilitate different levels and actors of governance to function in a coordinated and cooperative manner.
Containing health crises is a testimony of functional relationships among orders of the governments as public health transcends the arbitrary political boundaries created for administrative purposes. Such expansions would require the public authorities to find ways to define and exercise both formal and informal mechanisms to remove barriers, intensify information flow, appreciate collaborative leadership, and promote interagency relations. In a multi-level government, the lower-order governments, particularly the local governments, serve as the first responder to public demands (Morphet, 2008; Acharya, 2018) through frontline delivery (Pokharel & Sapkota, 2021). The roles of local governments in dealing with COVID have been largely appreciated in many countries, as they have taken decisive roles to apply national policy standards in the local contexts (Democracy Resource Center Nepal, 2020; Silva, 2022). However, a relevant aspect to understand in the practice of multi-level governance is ‘how did the intergovernmental relations function in managing the health crisis?’, which is the central theme of this paper. The case from Nepal would advantage global readers owing to the nature of political, economic, and social transition propelled by new experimentation of governance structure.
For setting the context of Nepal’s overall healthcare governance, this paper provides the country context, disaster risk profile, health management system, survey introduction, and key findings of the study in a coherent framework.
Political economy background
Nepal has survived natural, social, economic, and political crises in the past. Situated between the world’s two big economies and populations, China and India, it is accelerating the institutionalization of stable governance and economic development. The political crisis of the recent past, a decade-long armed conflict between 1996-2006, and political maneuvering led to the introduction of a new Constitution in 2015. This Constitution transformed Nepal from a unitary centralized form of governance to a decentralized federal system. It also ended the conventional monarchical system with the adoption of the republic system. This new polity has allocated government business among three tiers- federal, provincial, and local- of government with defined responsibilities (exclusive and concurrent). The new governance arrangements have allowed Nepal to function in a more concerted and complementary way to deal with public problems, with sub-national governments having autonomy in several functions to deal with the issues in their jurisdictions. The governance of Nepal is now managed by 761 governing units (federation, 7 provinces, and 753 local units), each order having defined roles, but overlapping in some cases. Health is an example of such overlap.
With the new governance architecture in place, the three orders of the governments are taking initiatives to implement constitutional mandates. The Constitution safeguards the autonomy of federal units while qualifying the model of intergovernmental relationships based on the principles of ‘cooperation, co-existence, and coordination’. It implies that the federal units have to adhere to the basic principles of cooperative federalism while implementing the constitutional mandates (Dhungana, Pokharel, & Poudel, 2021). Such cooperation may be both formal or informal and vertical or horizontal. For the effective functioning of the federal units, the Constitution and subsequent legal arrangements propose several structural and institutional arrangements for promoting intergovernmental relations including fiscal relations (Pokharel & Sapkota, 2021).
Intergovernmental relations
The theories and literature do not have a universal definition of intergovernmental relations. However, they acknowledge the diversity in basic structures, mechanisms, and institutionalization (Poirier & Saunders, 2010), a common purpose is clear- mechanisms, institutions, and opportunities for interactions among the orders of government. It has mainly two dimensions- structural and functional. While the structural dimension is about the institutional arrangements defined by the policies and laws that provide official space for interactions among the levels of government, the functional perspective assumes to be organic and evolving. The governing units may explore and agree on the areas of cooperation, exchange support and provide the best compliments to deal with the issues of 'interdependencies and spill-over effects due to overlaps in functions and jurisdictions' (McEwen, Petersohn, & Swan, 2015).
The national government may be interested to use coordination mechanisms to make sure that its policies and standards are implemented by the sub-national governments, while the sub-national governments may take it as a space to negotiate power and finance. In an institutionalized system, the defined frameworks and practices provide inputs for intergovernmental relations and are more official in processes and contents. However, there are limits to formal relations. The constitution, legislation, and policies are closed documents while the relationship is fluid and dynamic. To deal with inter-jurisdictional dynamism, informal means of interaction, communication, and engagement are equally important, given that such practices would promote the public interests and are then backed up by a formal process. In the absence of an institutionalized system, the relations are person-centric, ad-hoc, intuitive, and non-transparent. It also lacks accountability among the actors.
As Nepal is at the early stage of institutionalizing the three-tier federal system, assessing the dynamics of intergovernmental relations merits attention for two reasons. First, as Nepal’s federal form of governance is unfolding, it adds value to understanding to what extent the formal structural arrangements of intergovernmental interactions are functional. Second, public health is a shared responsibility among the levels of government, demanding a concerted collaboration among the government spheres. It is worthwhile to weigh and expose gaps in the practice of cooperation and coordination while dealing with the COVID-19 pandemic. This paper, therefore, contributes to updating the literature on intergovernmental relations through fresh insights of practices drawing lessons from a country that is undergoing political and governance transition.
Disaster and health pandemic profile
Nepal is also considered a country in the high-risk zone for disasters such as earthquakes, floods, landslides, climate-induced disasters, and health pandemics. The recent earthquake of 2015 claimed the lives of nearly 10,000 people and caused an economic loss of over $7 billion, almost one-third of GDP (National Planning Commission [NPC], 2015). Table 1 shows the major disaster risks in Nepal. In addition, Nepal suffers several disease outbreaks of different scales owing to poor socio-economic status, insufficient health infrastructures, and inefficiency of health governance. For example, in 2009 an outbreak of cholera was identified in over 30,000 people with a casualty of over 500 in a western uphill district of Jajarkot (Bhandari, Dixit, Ghimire, & Maskey, 2010). The district falls into a category of low human development index of the total of 77 districts in the country. A recent outbreak in the mid-western southern plain district of Kapilvastu[1] is another piece of evidence to reiterate that Nepal is in the risk zone of a health epidemic.
Table 1. Disaster Risk Profile of Nepal
Nepal is at the 107th position of 195 countries in the Global Health Security Index 2021, a global comparative index that measures the status of health governance in the aftermath of the COVID-19 pandemic (Bell & Nuzzo, 2021). The index provides estimates on six categories of COVID management - prevention, detection and reporting, rapid response, health system, commitments to improving national capacity, financing, and global norms, and risk environment. Among others, the report further highlights two critical issues for dealing with a health crisis: a) insufficient health capacity and b) ineffective coordination among national entities and global organizations. Nepal’s rank is below the global average, indicating potential gaps in the institutional capacity of managing health crises. Considering the constrained healthcare capacity, this paper aims to explore the functioning of the newly implemented federal governance structure of Nepal following the promulgation of the Constitution of Nepal in 2015, particularly from the perspective of coordination among the orders of the governments.
The COVID-19 pandemic has forced all countries, especially the low- and middle-income countries that have a poor health governance system, to assess their health governance capacities and take necessary steps to be prepared for a better future. For a developing country like Nepal, surviving the crisis is always a social, political, economic, governance, and policy issue. This paper focuses on the aspects of intergovernmental relations for managing the health crisis.
Nepal is practicing three-tier multi-level governance with each level having constitutionally enumerated competencies including the management of health services. As the new governance architecture replaced the unitary form of governance with a devolved federal structure, the transition was accelerating, and Nepal was struggling to institutionalize the constitutional provisions by installing governance structures and procedures (Thapa, Bam, Tiwari, Sinha, & Dahal, 2019). Meanwhile, COVID-19 emerged as a real assessment of the country's capacity to deal with the crisis. Considering that public health is a shared responsibility among the levels of government, the theory of intergovernmental relations underscores effective interactions among the governing units are vital in delivering services efficiently. Such interactions should be defined by processes and institutions (Phillimore, 2013) that would facilitate different levels and actors of governance to function in a coordinated and cooperative manner.
Containing health crises is a testimony of functional relationships among orders of the governments as public health transcends the arbitrary political boundaries created for administrative purposes. Such expansions would require the public authorities to find ways to define and exercise both formal and informal mechanisms to remove barriers, intensify information flow, appreciate collaborative leadership, and promote interagency relations. In a multi-level government, the lower-order governments, particularly the local governments, serve as the first responder to public demands (Morphet, 2008; Acharya, 2018) through frontline delivery (Pokharel & Sapkota, 2021). The roles of local governments in dealing with COVID have been largely appreciated in many countries, as they have taken decisive roles to apply national policy standards in the local contexts (Democracy Resource Center Nepal, 2020; Silva, 2022). However, a relevant aspect to understand in the practice of multi-level governance is ‘how did the intergovernmental relations function in managing the health crisis?’, which is the central theme of this paper. The case from Nepal would advantage global readers owing to the nature of political, economic, and social transition propelled by new experimentation of governance structure.
For setting the context of Nepal’s overall healthcare governance, this paper provides the country context, disaster risk profile, health management system, survey introduction, and key findings of the study in a coherent framework.
Political economy background
Nepal has survived natural, social, economic, and political crises in the past. Situated between the world’s two big economies and populations, China and India, it is accelerating the institutionalization of stable governance and economic development. The political crisis of the recent past, a decade-long armed conflict between 1996-2006, and political maneuvering led to the introduction of a new Constitution in 2015. This Constitution transformed Nepal from a unitary centralized form of governance to a decentralized federal system. It also ended the conventional monarchical system with the adoption of the republic system. This new polity has allocated government business among three tiers- federal, provincial, and local- of government with defined responsibilities (exclusive and concurrent). The new governance arrangements have allowed Nepal to function in a more concerted and complementary way to deal with public problems, with sub-national governments having autonomy in several functions to deal with the issues in their jurisdictions. The governance of Nepal is now managed by 761 governing units (federation, 7 provinces, and 753 local units), each order having defined roles, but overlapping in some cases. Health is an example of such overlap.
With the new governance architecture in place, the three orders of the governments are taking initiatives to implement constitutional mandates. The Constitution safeguards the autonomy of federal units while qualifying the model of intergovernmental relationships based on the principles of ‘cooperation, co-existence, and coordination’. It implies that the federal units have to adhere to the basic principles of cooperative federalism while implementing the constitutional mandates (Dhungana, Pokharel, & Poudel, 2021). Such cooperation may be both formal or informal and vertical or horizontal. For the effective functioning of the federal units, the Constitution and subsequent legal arrangements propose several structural and institutional arrangements for promoting intergovernmental relations including fiscal relations (Pokharel & Sapkota, 2021).
Intergovernmental relations
The theories and literature do not have a universal definition of intergovernmental relations. However, they acknowledge the diversity in basic structures, mechanisms, and institutionalization (Poirier & Saunders, 2010), a common purpose is clear- mechanisms, institutions, and opportunities for interactions among the orders of government. It has mainly two dimensions- structural and functional. While the structural dimension is about the institutional arrangements defined by the policies and laws that provide official space for interactions among the levels of government, the functional perspective assumes to be organic and evolving. The governing units may explore and agree on the areas of cooperation, exchange support and provide the best compliments to deal with the issues of 'interdependencies and spill-over effects due to overlaps in functions and jurisdictions' (McEwen, Petersohn, & Swan, 2015).
The national government may be interested to use coordination mechanisms to make sure that its policies and standards are implemented by the sub-national governments, while the sub-national governments may take it as a space to negotiate power and finance. In an institutionalized system, the defined frameworks and practices provide inputs for intergovernmental relations and are more official in processes and contents. However, there are limits to formal relations. The constitution, legislation, and policies are closed documents while the relationship is fluid and dynamic. To deal with inter-jurisdictional dynamism, informal means of interaction, communication, and engagement are equally important, given that such practices would promote the public interests and are then backed up by a formal process. In the absence of an institutionalized system, the relations are person-centric, ad-hoc, intuitive, and non-transparent. It also lacks accountability among the actors.
As Nepal is at the early stage of institutionalizing the three-tier federal system, assessing the dynamics of intergovernmental relations merits attention for two reasons. First, as Nepal’s federal form of governance is unfolding, it adds value to understanding to what extent the formal structural arrangements of intergovernmental interactions are functional. Second, public health is a shared responsibility among the levels of government, demanding a concerted collaboration among the government spheres. It is worthwhile to weigh and expose gaps in the practice of cooperation and coordination while dealing with the COVID-19 pandemic. This paper, therefore, contributes to updating the literature on intergovernmental relations through fresh insights of practices drawing lessons from a country that is undergoing political and governance transition.
Disaster and health pandemic profile
Nepal is also considered a country in the high-risk zone for disasters such as earthquakes, floods, landslides, climate-induced disasters, and health pandemics. The recent earthquake of 2015 claimed the lives of nearly 10,000 people and caused an economic loss of over $7 billion, almost one-third of GDP (National Planning Commission [NPC], 2015). Table 1 shows the major disaster risks in Nepal. In addition, Nepal suffers several disease outbreaks of different scales owing to poor socio-economic status, insufficient health infrastructures, and inefficiency of health governance. For example, in 2009 an outbreak of cholera was identified in over 30,000 people with a casualty of over 500 in a western uphill district of Jajarkot (Bhandari, Dixit, Ghimire, & Maskey, 2010). The district falls into a category of low human development index of the total of 77 districts in the country. A recent outbreak in the mid-western southern plain district of Kapilvastu[1] is another piece of evidence to reiterate that Nepal is in the risk zone of a health epidemic.
Table 1. Disaster Risk Profile of Nepal
Types of hazards |
Nature |
Location |
Reasons of vulnerability |
Landslides |
Recurrent |
The hilly districts of Nepal are located in the Siwalik, Mahabharat range (east-west lower hill range), mid-land, and also fore and higher Himalayas |
Both natural and human factors such as steep slopes, fragile geology, high intensity of rainfall, deforestation, and unplanned human settlements |
Floods |
Most common |
River basins like Koshi (eastern Nepal), Narayani (central), Karnali (mid-western), Mahakali (far-western) rivers perennial rivers |
Anthropogenic activities like improper land use, encroachment into vulnerable land slopes, and unplanned development activities such as the construction of roads and irrigation canals without proper protection measures in the vulnerable mountain belt and climate change |
Glacier lakes outburst floods (GLOFs) |
Occasional |
High altitude areas particularly on the foothill of the mountain |
Damming in by moraines, the lakes contained huge volumes of water melting off the glacier may lead to outbreak the lakes |
Earthquake |
Occasional |
Major active faults in east-west alignment, entire Nepal which lies in active seismic zone |
Siwalik, the lesser Himalaya and frontal part of the Higher Himalaya |
Fire |
Recurrent |
Mid hill areas |
78% of agro-base households, cluster-based houses more susceptible to catching fire, in dry season wild or forest fire |
Drought |
Recurrent |
Some parts of Terai, mid-land and Trans-Himalayan belts of Nepal |
Mostly caused by uneven and irregular low monsoon rainfall and the lack of irrigation facilities further exacerbates the effect of drought causing enormous loss of crops production leading to the shortage and insecurity of food |
Avalanche |
Occasional |
High mountainous region having rugged and steep slopes topographically |
Slopes, the thickness of snow, or human activity with cumulated debris in the snowline. |
Source: Ministry of Home Affairs (MoHA), 2017
Throughout the modern history of healthcare management, Nepal has survived the health crisis that took the lives of hundreds of thousands together with devastating socio-economic impact. These causes of death have differential impacts on the population depending on their socio-economic vulnerabilities (Pokharel & Dahal, 2020). However, in the past two decades, Nepal has made progress in combating the health crisis, thereby improving overall health governance. Between 1 January to 31 December 2021, the following 10 major causes of death are identified in Nepal, excluding natural disasters.
Table 2. Top 10 Causes of Death (health and road safety related) Between 1 January-31 December 2021
Throughout the modern history of healthcare management, Nepal has survived the health crisis that took the lives of hundreds of thousands together with devastating socio-economic impact. These causes of death have differential impacts on the population depending on their socio-economic vulnerabilities (Pokharel & Dahal, 2020). However, in the past two decades, Nepal has made progress in combating the health crisis, thereby improving overall health governance. Between 1 January to 31 December 2021, the following 10 major causes of death are identified in Nepal, excluding natural disasters.
Table 2. Top 10 Causes of Death (health and road safety related) Between 1 January-31 December 2021
Cause |
Number of deaths |
Coronary heart disease |
34,073 |
Stroke |
16,158 |
Lung disease |
13,815 |
Diarrheal diseases |
9,807 |
Influenza and pneumonia |
9,685 |
COVID-19 |
8,880 |
Diabetes mellitus |
6,537 |
Tuberculosis |
6,481 |
Road traffic accidents |
5,101 |
Source: World Life Expectancy, 2022
As displayed in Table 2, Nepal suffers from several health risks. Although the burden of non-communicable diseases is increasing, the contribution of communicable diseases including COVID was significant in the reference period. As communicable diseases transcend physical boundaries, it merits the attention of the orders of the government to strengthen coordination for combating these public health issues.
2. Healthcare governance in Nepal
Policy provisions and challenges of transition
Healthcare governance is one of the largest governance networks in Nepal. In the erstwhile system, the central government led by the Ministry of Health and Population was responsible for policy, regulation, finance, and management of health professionals. Nepal introduced the first fifteen-year long-term health plan in 1975. Much about the implementation status of the plan has been undocumented but evidence shows that the plan was instrumental to develop the foundation of health services in Nepal. Against this backdrop, the first National Health Policy was introduced in 1991, with one of the objectives to develop sub-national health capacity by establishing primary health centers and health posts as the frontline health service organizations. Amidst the criticisms of ineffective implementation of policy, Nepal introduced the second long-term health plan (1997-2017), intending to modernize health services and ensure universal access to healthcare. Following the promulgation of the Constitution of Nepal in 2015, an updated health policy reflecting the constitutional mandate that recognizes health as a fundamental right has been enforced in 2019.
The 2019 policy considers ‘healthy, alert and conscious citizens oriented to happy life’ as the overarching vision. The policy states to focus on the ‘integrated preparedness and response measures shall be adopted to combat communicable diseases, insect-borne and animal-borne diseases, problems related with climate change, other diseases, epidemics and disasters’ (Ministry of Health and Population [MoHP], 2019). However, the policy fails to address exclusively the intergovernmental dynamics of health crisis management and emergency services. The policy requires it to be updated to address the issues of health crisis management that surfaced during the outbreak of COVID-19.
Considering the wider scope and externalities of health services, the Constitution of Nepal 2015 has assigned health as a shared responsibility among the federal, provincial, and local governments. The division of functions is mainly based on the ‘principle of subsidiarity’ and the corresponding principle of ‘economies of scale’. With these principles, the local governments are mainly responsible for managing the basic health services, preventive measures through promotional activities, disease surveillance, and feeding data to the national system. In addition, they complement and support federal and provincial health programs. The provincial governments, being the medium-order government, are responsible for medium-order health services including provincial health policy, management of health facilities, developing the capacity of local governments, disease surveillance, receiving data from local governments, and feeding to the central database. The federal government, being the higher-order government, is responsible for national health policies, the management of tertiary and referral hospitals, control and management of communicable diseases, health financing, vaccination, and national health campaigns. While there are exclusive competences of levels of government, there are also considerable overlaps in mandates of healthcare services (Acharya, Upadhyay, & Acharya, 2020), creating confusion over sharing of responsibility.
Table 3. Allocation of Health Functions Among Federal, Provincial and Local Level
As displayed in Table 2, Nepal suffers from several health risks. Although the burden of non-communicable diseases is increasing, the contribution of communicable diseases including COVID was significant in the reference period. As communicable diseases transcend physical boundaries, it merits the attention of the orders of the government to strengthen coordination for combating these public health issues.
2. Healthcare governance in Nepal
Policy provisions and challenges of transition
Healthcare governance is one of the largest governance networks in Nepal. In the erstwhile system, the central government led by the Ministry of Health and Population was responsible for policy, regulation, finance, and management of health professionals. Nepal introduced the first fifteen-year long-term health plan in 1975. Much about the implementation status of the plan has been undocumented but evidence shows that the plan was instrumental to develop the foundation of health services in Nepal. Against this backdrop, the first National Health Policy was introduced in 1991, with one of the objectives to develop sub-national health capacity by establishing primary health centers and health posts as the frontline health service organizations. Amidst the criticisms of ineffective implementation of policy, Nepal introduced the second long-term health plan (1997-2017), intending to modernize health services and ensure universal access to healthcare. Following the promulgation of the Constitution of Nepal in 2015, an updated health policy reflecting the constitutional mandate that recognizes health as a fundamental right has been enforced in 2019.
The 2019 policy considers ‘healthy, alert and conscious citizens oriented to happy life’ as the overarching vision. The policy states to focus on the ‘integrated preparedness and response measures shall be adopted to combat communicable diseases, insect-borne and animal-borne diseases, problems related with climate change, other diseases, epidemics and disasters’ (Ministry of Health and Population [MoHP], 2019). However, the policy fails to address exclusively the intergovernmental dynamics of health crisis management and emergency services. The policy requires it to be updated to address the issues of health crisis management that surfaced during the outbreak of COVID-19.
Considering the wider scope and externalities of health services, the Constitution of Nepal 2015 has assigned health as a shared responsibility among the federal, provincial, and local governments. The division of functions is mainly based on the ‘principle of subsidiarity’ and the corresponding principle of ‘economies of scale’. With these principles, the local governments are mainly responsible for managing the basic health services, preventive measures through promotional activities, disease surveillance, and feeding data to the national system. In addition, they complement and support federal and provincial health programs. The provincial governments, being the medium-order government, are responsible for medium-order health services including provincial health policy, management of health facilities, developing the capacity of local governments, disease surveillance, receiving data from local governments, and feeding to the central database. The federal government, being the higher-order government, is responsible for national health policies, the management of tertiary and referral hospitals, control and management of communicable diseases, health financing, vaccination, and national health campaigns. While there are exclusive competences of levels of government, there are also considerable overlaps in mandates of healthcare services (Acharya, Upadhyay, & Acharya, 2020), creating confusion over sharing of responsibility.
Table 3. Allocation of Health Functions Among Federal, Provincial and Local Level
Federal level |
Provincial level |
Local level |
|
|
|
Source: Summarized from Constitution of Nepal 2015 and related acts
This transformation in health governance was effective from the 2015 Constitution and subsequent elections at local, provincial, and federal levels in 2017. Following the initial level of organizational set-up, Nepal is facing challenges to manage transition together with unclarity in the functional allocations, the complexity of the new system, and the residual impact of the erstwhile system (Pokharel & Sapkota, 2021; Dhungana, Pokharel, & Poudel, 2021), the COVID pandemic imposed additional burden to Nepal’s ongoing transition. Nepal's adventure with the federal system was to be supported by immediate and effective arrangements of policies, legislation, and structures. Although the Constitution provides a broader guideline for business allocation among the orders of government, the centrally managed functions and functionaries were required to transfer to subnational governments through a clearly defined allocation framework.
In the absence of such a framework, there was an unanticipated delay in setting up new arrangements and facilitating the transition. As healthcare governance is one of the major public activities, having a large network of facilities, and financial and human resources, the restructuring was a daunting task. The transition witnessed challenges to ensure uninterrupted health services and medical supplies (Thapa, Bam, Tiwari, Sinha, & Dahal, 2019). While the debates on constitutional mandates versus legacy among federal, provincial, and local governments in ownership and control of health facilities and services were enduring, COVID-19 confronted the wobbling healthcare governance.
Health financing
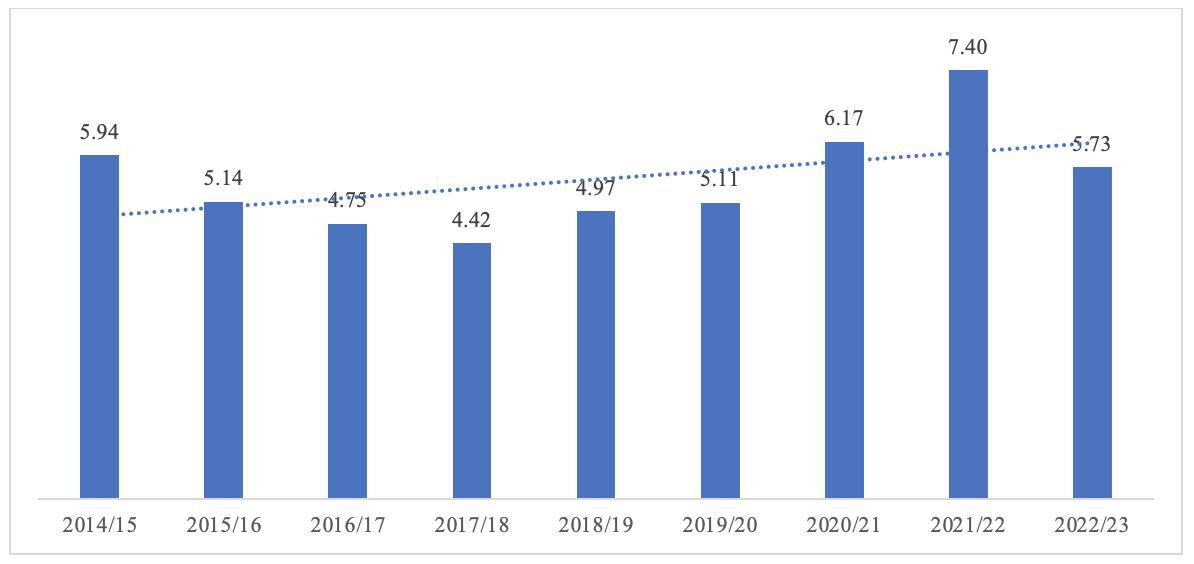
The federal budget is the main source of health sector financing. Nepal's health financing is far less (4.45% of GDP) than the world's average of 9.83% of GDP in 2019 (The World Bank, 2022). Figure 1 shows the allocation percentage in the health sector in the national budget between 2014/15 to 2022/23. The highest allocation in the health sector was in 2021/22, owing to the government's allocation priority to contain COVID, then a reduction in the subsequent year. However, on average, the health sector has received around 5% of the total budget in the last decade, which is far less than the WHO recommendation.
Figure 1. Proportion of Allocation in the Health Sector in the Federal Budget (2014/15-2022/23)
This transformation in health governance was effective from the 2015 Constitution and subsequent elections at local, provincial, and federal levels in 2017. Following the initial level of organizational set-up, Nepal is facing challenges to manage transition together with unclarity in the functional allocations, the complexity of the new system, and the residual impact of the erstwhile system (Pokharel & Sapkota, 2021; Dhungana, Pokharel, & Poudel, 2021), the COVID pandemic imposed additional burden to Nepal’s ongoing transition. Nepal's adventure with the federal system was to be supported by immediate and effective arrangements of policies, legislation, and structures. Although the Constitution provides a broader guideline for business allocation among the orders of government, the centrally managed functions and functionaries were required to transfer to subnational governments through a clearly defined allocation framework.
In the absence of such a framework, there was an unanticipated delay in setting up new arrangements and facilitating the transition. As healthcare governance is one of the major public activities, having a large network of facilities, and financial and human resources, the restructuring was a daunting task. The transition witnessed challenges to ensure uninterrupted health services and medical supplies (Thapa, Bam, Tiwari, Sinha, & Dahal, 2019). While the debates on constitutional mandates versus legacy among federal, provincial, and local governments in ownership and control of health facilities and services were enduring, COVID-19 confronted the wobbling healthcare governance.
Health financing
The federal budget is the main source of health sector financing. Nepal's health financing is far less (4.45% of GDP) than the world's average of 9.83% of GDP in 2019 (The World Bank, 2022). Figure 1 shows the allocation percentage in the health sector in the national budget between 2014/15 to 2022/23. The highest allocation in the health sector was in 2021/22, owing to the government's allocation priority to contain COVID, then a reduction in the subsequent year. However, on average, the health sector has received around 5% of the total budget in the last decade, which is far less than the WHO recommendation.
Figure 1. Proportion of Allocation in the Health Sector in the Federal Budget (2014/15-2022/23)
Source: Collected from annual budget speech (2014/15-2022/23) from Ministry of Finance [MoF] (2022)
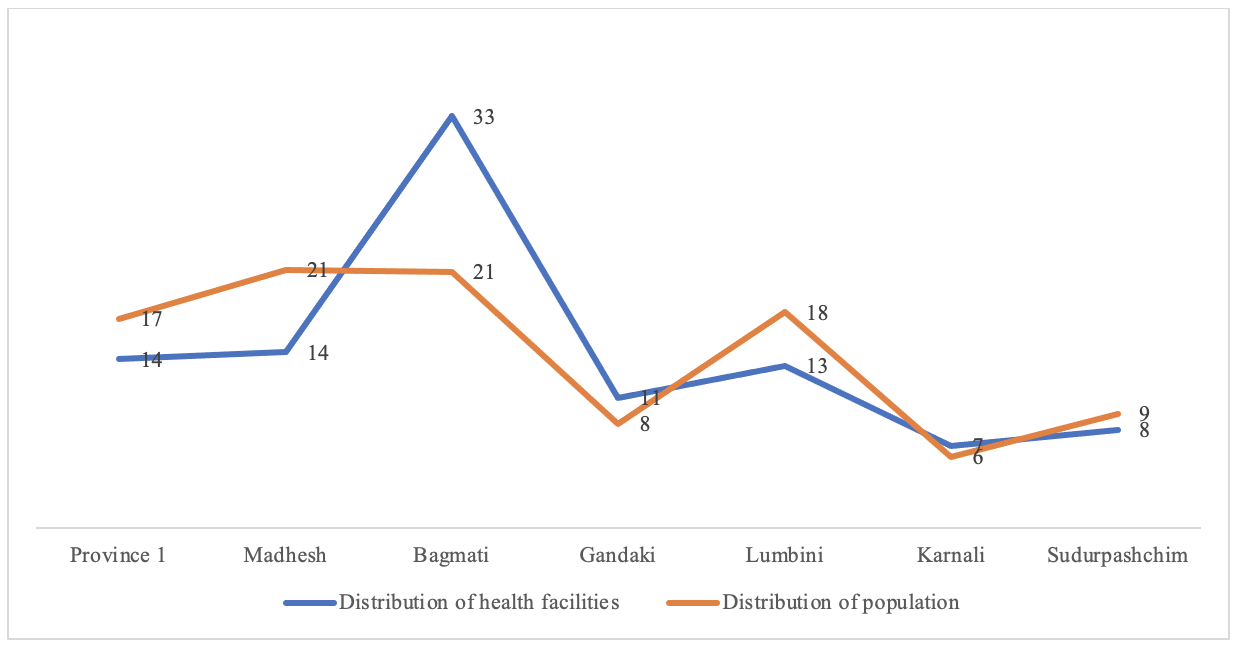
The data of the Department of Health Services shows as of 2017/18 nearly 7,000 health facilities of different types form the institutional structure of health governance. Of these, nearly 30% are private health facilities providing health services throughout the country. However, a noticeable disparity is observed in terms of the distribution of health facilities with the ratio of population distribution. For example, Bagmati Province, which also includes the federal capital, has domination in the distribution of health facilities, with nearly 35% of total health facilities against a one-fifth share of the total population. On the contrary, Madhesh Province holds 14% of health facilities against an equivalent share with Bagmati Province in the total population. This disparity warrants a foreseeable capacity gap in healthcare governance and calls for balancing the distribution of health facilities in response to population distribution.
Figure 2. Distribution of Health Facilities and Population by Provinces of Nepal
The data of the Department of Health Services shows as of 2017/18 nearly 7,000 health facilities of different types form the institutional structure of health governance. Of these, nearly 30% are private health facilities providing health services throughout the country. However, a noticeable disparity is observed in terms of the distribution of health facilities with the ratio of population distribution. For example, Bagmati Province, which also includes the federal capital, has domination in the distribution of health facilities, with nearly 35% of total health facilities against a one-fifth share of the total population. On the contrary, Madhesh Province holds 14% of health facilities against an equivalent share with Bagmati Province in the total population. This disparity warrants a foreseeable capacity gap in healthcare governance and calls for balancing the distribution of health facilities in response to population distribution.
Figure 2. Distribution of Health Facilities and Population by Provinces of Nepal
Source: Ministry of Health and Population [MoHP], (2018); Central Bureau of Statistics (2022)
3. COVID Management: Policies and Institutional Arrangements
The first COVID case in Nepal was detected on 23 January 2020. Following the detection, Nepal saw a slow spread of COVID at the early stage. The peak of the first wave was noticed only in the third week of October 2020, nine months later, with a record of 5,753 cases on 21 October 2020. The second wave emerged in April 2021, which was more devastating than the first wave as observed worldwide. The second wave alone contributed to more than 80% of total infections and 90% of total deaths in Nepal. The COVID positivity rate in the second wave was higher than 2.5 times that of the first wave. For a specific day, the positivity rate in the second wave scaled to over half of the total tests against 35%in the first wave (Ghimire, 2021). The cumulative data shows as of 8 May 2022, Nepal has 978,942 COVID cases with 98.8% recovery and cumulative deaths of 11,952 with a rate of 1.2%.[1] In terms of vaccination, Nepal is mainly dependent on grants, purchases, and the Covax scheme. As of 8 May 2022, almost 66% of the eligible population have received a complete vaccination and 8.9% have full doses, ranking in the 5th position in the SAARC region and seven percentage points higher coverage than the global average[2].
With the detection of the first case and global news of the outbreak including in the neighboring countries, Nepal took official initiatives to combat the pandemic by forming a High-Level Coordination Committee (HLCC) in early March 2020 and made attempts to mobilize all concerned sectors. The HLCC was then made responsible for making decisions and coordination among all the stakeholders including the provincial and local governments. The HLCC was eventually replaced by the COVID-19 Crisis Management Centre (CCMC), which had clear mandates. The CCCM was vertically organized with a similar structure replicated at provincial, district, and municipal levels, but no vertical structural linkages amongst them. The unilateral decisions of CCMC were circulated downward. The sub-national governments were considered passive agencies of the federal decisions.
During the first wave, the government made attempts to address the COVID crisis through executive orders rather than any well-framed legal and policy instruments, while there were several guidelines and procedures introduced to contain the crisis. In the second wave of COVID, the government introduced COVID-19 Crisis Management Ordinance on 20 May 2021, which gave a legal mandate to COVID-19 Crisis Management Centre (CCMC) to take decisions in combating the crisis. However, the ordinance could not get approval from the parliament, reinstating the practices of the decision process to executive orders.
In the early days, the CCMC used to meet regularly, make decisions and resolve issues of coordination, but gradually it became ineffective. The agencies involved in managing COVID started working in their way. The decisions of the CCMC were ignored by the Cabinet and other responsible agencies, making COVID control efforts disintegrated and departmental. The Ministry of Health and Population, the focal agency to deal with public health issues, considered the CCMC as irrelevant and just an additional structure having no functional relevance (Bagale, 2020). The declining effectiveness of the CCMC was mainly due to unclear division of work and undermining of the strengths of the regular structure, particularly of the Ministry of Health and Population. Eventually, the much-overvalued body was considered a burden (Pradhan & Prasain, 2021).
Although the federal government was decisive in managing the COVID crisis, the provincial and local governments were mainly made responsible for public health service delivery, prevention of transmission and epidemiological investigations and tracking, ensuring other public services, and supporting social and relief activities (Mainali, Tosun, & Yilmaz, 2021). In addition, the sub-national governments were made responsible to implement federal orders and deal with public grievances, maintain records of the immigrants and other beneficiaries, distribute relief packages, and promote public health awareness.
4. Local Government and Pandemic Management
This section presents the findings from the survey of the local governments. The survey mainly captures the perspective of the local governments on the dimensions of COVID control activities, financial arrangements, policy, and political coordination among the orders of the governments. For making comparison over the periods, this paper draws results from the Round 1 survey conducted in May-June 2020 (sample of 115 LGs of the 753) and Round 2 survey conducted in October-November 2020 (sample of 115 LGs of the 753), and Round 3 survey conducted in April-May 2021 (census of all 753 LGs). The samples LGs in Round I and Round II were a replication of the Federalism Capacity Needs Assessment study conducted by Georgia State University and Nepal Administrative Staff College for the Government of Nepal in 2019.[1] The study used multi-stage stratified random sampling to make the sample representative of Nepal’s local governments, while Round 3 was a census of all local governments. The survey respondents were the elected chiefs (mayor of urban municipality and chairperson of the rural municipality), deputy chief, and chief administrative officer of the local governments. This paper uses responses from the elected chiefs only. This survey was jointly conducted by a team of Yale Economic Growth Center, London School of Economics and Political Sciences, Governance Lab and Nepal Administrative Staff College. Data were collected using a semi-structured questionnaire that was administered through telephone interviews in a strictly regulated protocol.
How did local governments respond to COVID?
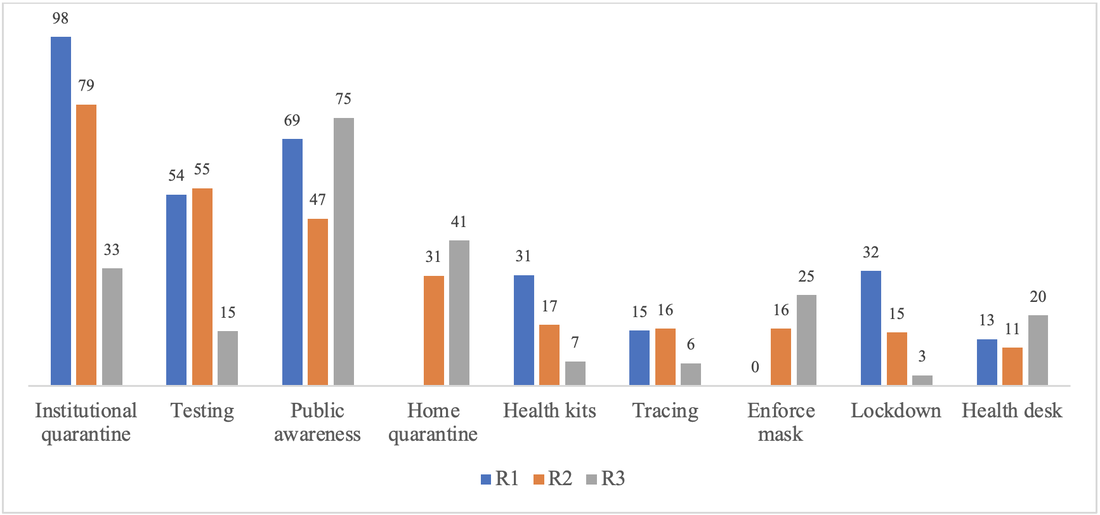
Local governments have been involved in several public health activities of preventive and curative services. Management of quarantine, testing, tracing, management of home quarantine, distributing health kits, enforcing a mask and other social measures, lockdown, and health desk were the major activities that local governments identified themselves that they were involved with. In the first round (May-June 2020), the local governments were actively involved in the management of quarantine (97.6%), public awareness (69.0%), and testing (53.6%). By October-November 2020, a decline in the engagement of local governments in some COVID-containing activities was observed. For example, 79% of local governments said to have been engaged in quarantine, 20 percentage points less than earlier round, while 55% were engaged in testing, slightly higher than the earlier round, and involvement in public awareness was reduced to 47%, almost 20 percentage points less than the earlier round. Importantly, management of home quarantine emerged as a new function as 31% of local governments reported to have been engaged to manage it. Likewise, enforcement of masks was an emerging priority for 16% of local governments, while 15% of local governments said to have been actively engaged in enforcing lockdown, almost 16 percentage points less than the earlier round.
The third round of the survey, corroborating the second wave of COVID, showed a different trend in the engagement of local governments. Engagement in management of institutional (a public center) quarantine further declined to 33%, testing had a sharp decline to 15%, while engagement in public awareness increased to 75%, management of home quarantine increased to 41%, 10 percentage points higher than the second round. Likewise, enforcement of masks (25.4%) and management of health desk (19.7%) were other priorities for the local governments.
In addition, management of schools, COVID hospitals, ambulance services, implementing social distancing, and administering vaccines were other emerging activities that local governments were found to be involved in the wake of the second wave.
Figure 3. Activities of Local Governments in COVID response (R1, R2, and R3)
3. COVID Management: Policies and Institutional Arrangements
The first COVID case in Nepal was detected on 23 January 2020. Following the detection, Nepal saw a slow spread of COVID at the early stage. The peak of the first wave was noticed only in the third week of October 2020, nine months later, with a record of 5,753 cases on 21 October 2020. The second wave emerged in April 2021, which was more devastating than the first wave as observed worldwide. The second wave alone contributed to more than 80% of total infections and 90% of total deaths in Nepal. The COVID positivity rate in the second wave was higher than 2.5 times that of the first wave. For a specific day, the positivity rate in the second wave scaled to over half of the total tests against 35%in the first wave (Ghimire, 2021). The cumulative data shows as of 8 May 2022, Nepal has 978,942 COVID cases with 98.8% recovery and cumulative deaths of 11,952 with a rate of 1.2%.[1] In terms of vaccination, Nepal is mainly dependent on grants, purchases, and the Covax scheme. As of 8 May 2022, almost 66% of the eligible population have received a complete vaccination and 8.9% have full doses, ranking in the 5th position in the SAARC region and seven percentage points higher coverage than the global average[2].
With the detection of the first case and global news of the outbreak including in the neighboring countries, Nepal took official initiatives to combat the pandemic by forming a High-Level Coordination Committee (HLCC) in early March 2020 and made attempts to mobilize all concerned sectors. The HLCC was then made responsible for making decisions and coordination among all the stakeholders including the provincial and local governments. The HLCC was eventually replaced by the COVID-19 Crisis Management Centre (CCMC), which had clear mandates. The CCCM was vertically organized with a similar structure replicated at provincial, district, and municipal levels, but no vertical structural linkages amongst them. The unilateral decisions of CCMC were circulated downward. The sub-national governments were considered passive agencies of the federal decisions.
During the first wave, the government made attempts to address the COVID crisis through executive orders rather than any well-framed legal and policy instruments, while there were several guidelines and procedures introduced to contain the crisis. In the second wave of COVID, the government introduced COVID-19 Crisis Management Ordinance on 20 May 2021, which gave a legal mandate to COVID-19 Crisis Management Centre (CCMC) to take decisions in combating the crisis. However, the ordinance could not get approval from the parliament, reinstating the practices of the decision process to executive orders.
In the early days, the CCMC used to meet regularly, make decisions and resolve issues of coordination, but gradually it became ineffective. The agencies involved in managing COVID started working in their way. The decisions of the CCMC were ignored by the Cabinet and other responsible agencies, making COVID control efforts disintegrated and departmental. The Ministry of Health and Population, the focal agency to deal with public health issues, considered the CCMC as irrelevant and just an additional structure having no functional relevance (Bagale, 2020). The declining effectiveness of the CCMC was mainly due to unclear division of work and undermining of the strengths of the regular structure, particularly of the Ministry of Health and Population. Eventually, the much-overvalued body was considered a burden (Pradhan & Prasain, 2021).
Although the federal government was decisive in managing the COVID crisis, the provincial and local governments were mainly made responsible for public health service delivery, prevention of transmission and epidemiological investigations and tracking, ensuring other public services, and supporting social and relief activities (Mainali, Tosun, & Yilmaz, 2021). In addition, the sub-national governments were made responsible to implement federal orders and deal with public grievances, maintain records of the immigrants and other beneficiaries, distribute relief packages, and promote public health awareness.
4. Local Government and Pandemic Management
This section presents the findings from the survey of the local governments. The survey mainly captures the perspective of the local governments on the dimensions of COVID control activities, financial arrangements, policy, and political coordination among the orders of the governments. For making comparison over the periods, this paper draws results from the Round 1 survey conducted in May-June 2020 (sample of 115 LGs of the 753) and Round 2 survey conducted in October-November 2020 (sample of 115 LGs of the 753), and Round 3 survey conducted in April-May 2021 (census of all 753 LGs). The samples LGs in Round I and Round II were a replication of the Federalism Capacity Needs Assessment study conducted by Georgia State University and Nepal Administrative Staff College for the Government of Nepal in 2019.[1] The study used multi-stage stratified random sampling to make the sample representative of Nepal’s local governments, while Round 3 was a census of all local governments. The survey respondents were the elected chiefs (mayor of urban municipality and chairperson of the rural municipality), deputy chief, and chief administrative officer of the local governments. This paper uses responses from the elected chiefs only. This survey was jointly conducted by a team of Yale Economic Growth Center, London School of Economics and Political Sciences, Governance Lab and Nepal Administrative Staff College. Data were collected using a semi-structured questionnaire that was administered through telephone interviews in a strictly regulated protocol.
How did local governments respond to COVID?
Local governments have been involved in several public health activities of preventive and curative services. Management of quarantine, testing, tracing, management of home quarantine, distributing health kits, enforcing a mask and other social measures, lockdown, and health desk were the major activities that local governments identified themselves that they were involved with. In the first round (May-June 2020), the local governments were actively involved in the management of quarantine (97.6%), public awareness (69.0%), and testing (53.6%). By October-November 2020, a decline in the engagement of local governments in some COVID-containing activities was observed. For example, 79% of local governments said to have been engaged in quarantine, 20 percentage points less than earlier round, while 55% were engaged in testing, slightly higher than the earlier round, and involvement in public awareness was reduced to 47%, almost 20 percentage points less than the earlier round. Importantly, management of home quarantine emerged as a new function as 31% of local governments reported to have been engaged to manage it. Likewise, enforcement of masks was an emerging priority for 16% of local governments, while 15% of local governments said to have been actively engaged in enforcing lockdown, almost 16 percentage points less than the earlier round.
The third round of the survey, corroborating the second wave of COVID, showed a different trend in the engagement of local governments. Engagement in management of institutional (a public center) quarantine further declined to 33%, testing had a sharp decline to 15%, while engagement in public awareness increased to 75%, management of home quarantine increased to 41%, 10 percentage points higher than the second round. Likewise, enforcement of masks (25.4%) and management of health desk (19.7%) were other priorities for the local governments.
In addition, management of schools, COVID hospitals, ambulance services, implementing social distancing, and administering vaccines were other emerging activities that local governments were found to be involved in the wake of the second wave.
Figure 3. Activities of Local Governments in COVID response (R1, R2, and R3)
R1= First round of survey between May-June 2020 (sample of 115 LGs)
R2= Second round of survey between October-November 2020 (sample of 115 LGs)
R3= Third round of survey between April-May 2021 (all 753 LGs)
Such a shift in activities of the local governments could be attributed to evolving nature of the pandemic- from preventive to curative. In the first wave, the focus was on prevention, where the local governments could play significant roles through quarantine, public awareness, and other social measures. In the second wave of COVID, the demand for curative services received higher priority, which was beyond the capacity and jurisdictions of the local governments. Further, asthe COVID pandemic prolonged, people applied health measures on their own, particularly in testing, quarantine, and other social measures.
Challenges faced by local governments in dealing with COVID
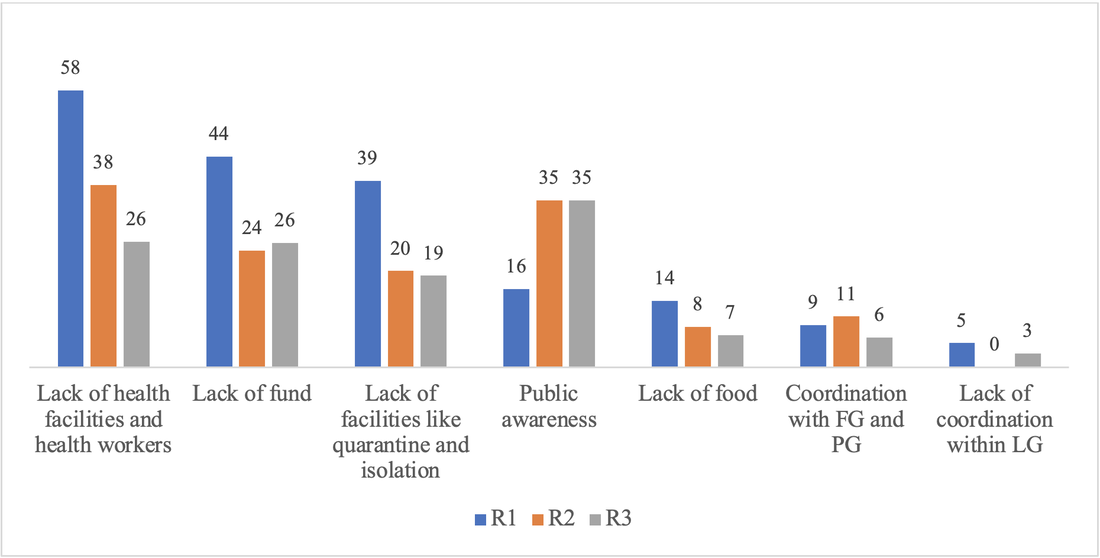
Further comparative analysis of challenges faced by the local governments to contain COVID shows a varied response over the periods. Inadequate health facilities and health workers were the common challenges that local governments identified throughout but in a declining trend. Noticeably, a decline in the proportion of LGs reporting a lack of health facilities and health workers was recorded at 20 percentage points between round 1 and round 2, and a further decline of 12 percentage points between round 2 and round 3. It may be because, during the crisis, the governments made interventions to improve health facilities, particularly in the expansion of testing centers, upgradation of health facilities, increasing the number of health workers, declaring COVID-specific hospitals, among others. Over the periods, health professionals extended their capacities, they were trained and motivated to deal with the crisis, the social stigma that was alarming at an early stage (Singh & Subedi, 2020) gradually disappeared, and health professionals’ capacity to cope with emergencies improved.
Figure 4. Challenges Faced by the Local Governments in Dealing with COVID
R2= Second round of survey between October-November 2020 (sample of 115 LGs)
R3= Third round of survey between April-May 2021 (all 753 LGs)
Such a shift in activities of the local governments could be attributed to evolving nature of the pandemic- from preventive to curative. In the first wave, the focus was on prevention, where the local governments could play significant roles through quarantine, public awareness, and other social measures. In the second wave of COVID, the demand for curative services received higher priority, which was beyond the capacity and jurisdictions of the local governments. Further, asthe COVID pandemic prolonged, people applied health measures on their own, particularly in testing, quarantine, and other social measures.
Challenges faced by local governments in dealing with COVID
Further comparative analysis of challenges faced by the local governments to contain COVID shows a varied response over the periods. Inadequate health facilities and health workers were the common challenges that local governments identified throughout but in a declining trend. Noticeably, a decline in the proportion of LGs reporting a lack of health facilities and health workers was recorded at 20 percentage points between round 1 and round 2, and a further decline of 12 percentage points between round 2 and round 3. It may be because, during the crisis, the governments made interventions to improve health facilities, particularly in the expansion of testing centers, upgradation of health facilities, increasing the number of health workers, declaring COVID-specific hospitals, among others. Over the periods, health professionals extended their capacities, they were trained and motivated to deal with the crisis, the social stigma that was alarming at an early stage (Singh & Subedi, 2020) gradually disappeared, and health professionals’ capacity to cope with emergencies improved.
Figure 4. Challenges Faced by the Local Governments in Dealing with COVID
R1= First round of survey between May-June 2020 (sample 115)
R2= Second round of survey between October-November 2020 (sample 115)
R3= Third round of survey between April-May 2021 (sample 753)
Other prominent challenges facing local governments were lack of funds, lack of facilities like quarantine and isolation, public awareness, lack of food for needy and vulnerable populations, and coordination with the federal and provincial governments. All challenges, as perceived by the local governments are on a declining trend but public awareness was on the increasing trend, indicating that educating the public was a challenge, having the cross-sectional impact of such apathy. Studies have shown considerable gaps between knowledge and practice of public safety measures, with lower practice against higher knowledge (Nepal Health Research Council [NHRC], 2020; Sah et al., 2022). Managing public movements at the borders and returnees has been an enduring challenge as Nepal has open and porous borders with India. It is estimated that over five million Nepalis are living in India while nearly one million Indians are in Nepal. The poorly regulated and sub-standard borders of Nepal and India are always busy for both entry and exit. The local governments, particularly adjoining Indian territory, confronted challenges to managing returnees. In addition, the local governments considered the distribution of vaccines as an emerging challenge in the third round.
Support and coordination with federal and provincial governments
A pandemic, such as COVID has an inter-jurisdictional spillover effect and requires competent intergovernmental support and coordination. Such collaboration would improve the enforcement of policy measures, delivery of services, and addressing public demands. However, the results show that in the perception of local governments, such support and coordination were largely insufficient. Important to note is that the local governments perceived that support and coordination have declined over the periods.
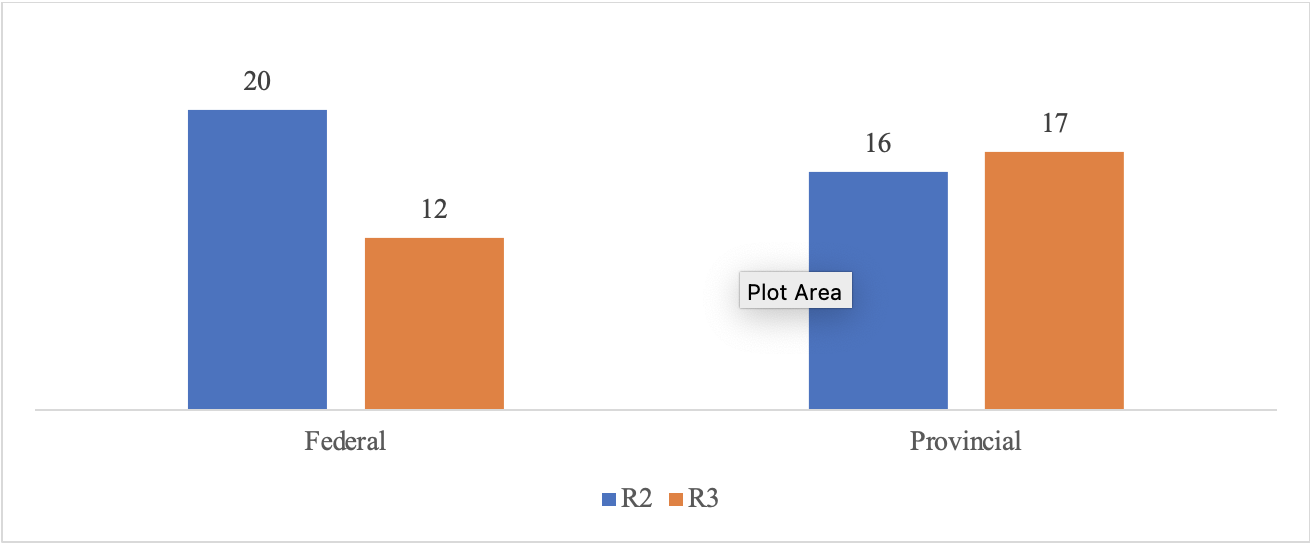
The support includes policy, financial, technical, and human resources while the coordination is more about information flow and decision process. In round 2, one-fifth of local governments considered the support from the federal government adequate while only 16% of local governments perceived so for the provincial governments. The proportion of the local governments considering adequate federal support further declined by eight percentage points in round 3, while it had a marginal increase with the provincial governments.
Figure 5. Proportion of Local Governments Reporting Adequate Support from Federal and Provincial Governments
R2= Second round of survey between October-November 2020 (sample 115)
R3= Third round of survey between April-May 2021 (sample 753)
Other prominent challenges facing local governments were lack of funds, lack of facilities like quarantine and isolation, public awareness, lack of food for needy and vulnerable populations, and coordination with the federal and provincial governments. All challenges, as perceived by the local governments are on a declining trend but public awareness was on the increasing trend, indicating that educating the public was a challenge, having the cross-sectional impact of such apathy. Studies have shown considerable gaps between knowledge and practice of public safety measures, with lower practice against higher knowledge (Nepal Health Research Council [NHRC], 2020; Sah et al., 2022). Managing public movements at the borders and returnees has been an enduring challenge as Nepal has open and porous borders with India. It is estimated that over five million Nepalis are living in India while nearly one million Indians are in Nepal. The poorly regulated and sub-standard borders of Nepal and India are always busy for both entry and exit. The local governments, particularly adjoining Indian territory, confronted challenges to managing returnees. In addition, the local governments considered the distribution of vaccines as an emerging challenge in the third round.
Support and coordination with federal and provincial governments
A pandemic, such as COVID has an inter-jurisdictional spillover effect and requires competent intergovernmental support and coordination. Such collaboration would improve the enforcement of policy measures, delivery of services, and addressing public demands. However, the results show that in the perception of local governments, such support and coordination were largely insufficient. Important to note is that the local governments perceived that support and coordination have declined over the periods.
The support includes policy, financial, technical, and human resources while the coordination is more about information flow and decision process. In round 2, one-fifth of local governments considered the support from the federal government adequate while only 16% of local governments perceived so for the provincial governments. The proportion of the local governments considering adequate federal support further declined by eight percentage points in round 3, while it had a marginal increase with the provincial governments.
Figure 5. Proportion of Local Governments Reporting Adequate Support from Federal and Provincial Governments
R1= First round of survey between May-June 2020 (sample 115). This question was not asked in round 1.
R2= Second round of survey between October-November 2020 (sample 115)
R3= Third round of survey between April-May 2021 (sample 753)
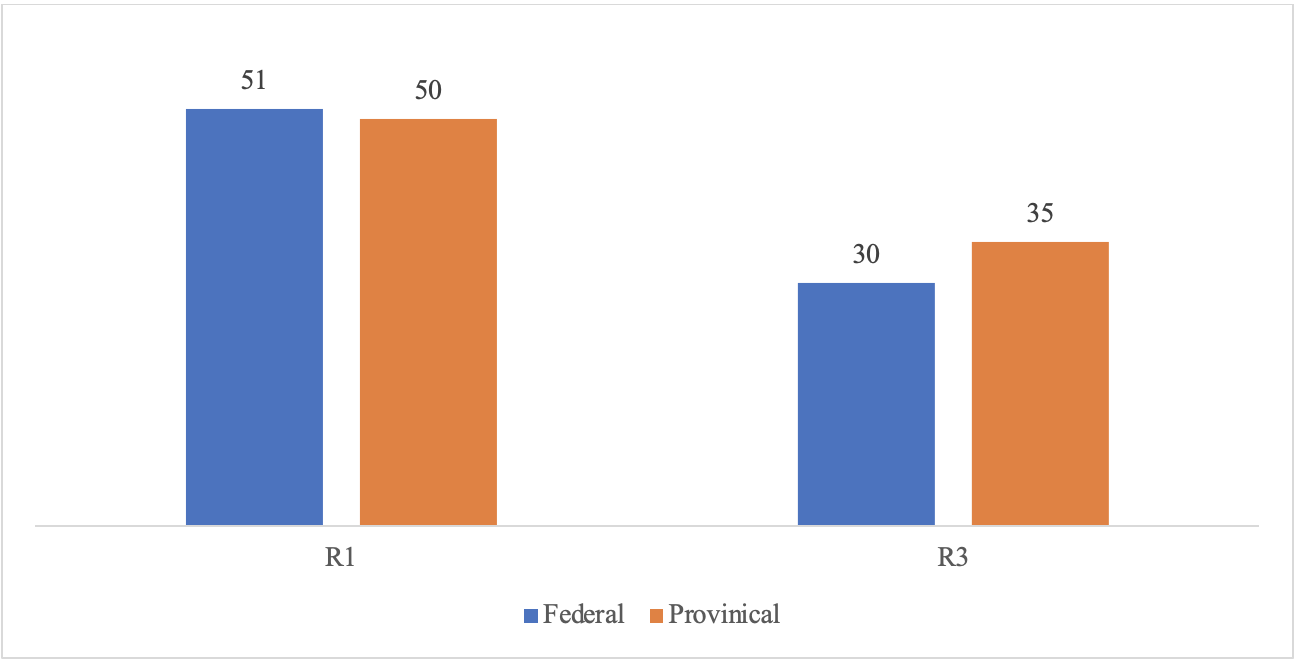
Similar, but relatively better for coordination compared to support, a serious gap in terms of intergovernmental coordination was observed. In round 1, almost half of the local governments perceived enough coordination with the federal and provincial governments, which declined dramatically in round 3 with 21 percentage points for the federal government and 15 percentage points for the provincial governments. Such a gap in the coordination may have negatively impacted the overall performance of managing the crisis.
Figure 6. Proportion of Local Governments Reporting Enough Coordination with the Federal and Provincial Governments
R2= Second round of survey between October-November 2020 (sample 115)
R3= Third round of survey between April-May 2021 (sample 753)
Similar, but relatively better for coordination compared to support, a serious gap in terms of intergovernmental coordination was observed. In round 1, almost half of the local governments perceived enough coordination with the federal and provincial governments, which declined dramatically in round 3 with 21 percentage points for the federal government and 15 percentage points for the provincial governments. Such a gap in the coordination may have negatively impacted the overall performance of managing the crisis.
Figure 6. Proportion of Local Governments Reporting Enough Coordination with the Federal and Provincial Governments
R1= First round of survey between May-June 2020 (sample 115).
R2= Second round of survey between October-November 2020 (sample 115). This question was not asked in round 2.
R3= Third round of survey between April-May 2021 (sample 753)
In addition, 35% of local governments in round 2 expressed some sort of disagreement in the ways that the federal government took decisions to deal with COVID, particularly in the issues of financing, lockdown, testing, tracing, quarantine, distribution of relief, and vaccines. The proportion of local governments reporting disagreement with the provincial government was slightly less than 30%. These disagreements were mainly in the way the federal government made decisions, the federal policies on lockdown, disproportionate sharing of financial resources (Bhandari, et al., 2020), medical support, distribution of medical supplies and vaccines, and deployment of health professionals. Sub-national governments have mainly criticized the tendency of unilateral decisions of the federal government to ignore the local context and requirements (Mainali, Tosun, & Yilmaz, 2021; Ghimire, 2021). The major deficit in pandemic control was the absence of the federal pandemic act. The CO VID response has been guided by the Infectious Disease Act 1964, the act which was functional in the erstwhile unitary system has been unresponsive to the federal structure. The Act does not recognize the roles of provincial and local governments but mandates agencies of the central government to exercise authority. Although the federal government introduced the COVID control ordinance in 2021, it failed to receive parliamentary approval, pushing COVID control back to half a century-old legislature, and causing lapses in intergovernmental relations.
On the other side, the inept functioning of provincial and local governments was equally responsible for ineffective vertical and horizontal coordination. Despite having low capacity, the local governments, as the first responder, played a relatively better role to contain the health crisis. The provincial governments, the medium order government having responsibility for providing leadership to local governments within their jurisdictions and negotiating with the federal government for effective delivery and leveraging backstopping for local governments and also having ownership of medium order hospitals, were largely criticized for their ineffective roles.
As Nepal's federal system is in its infancy, the structural arrangements to promote intergovernmental relations are yet to be institutionalized. Some coordination mechanisms such as the Inter-Provincial Council, National Coordination Councils, and other structures of coordination are provisioned in the Constitution and subsequent legislations, nonetheless, they are largely dysfunctional (Pokharel & Sapkota, 2021). The CCMC, a top-notch body to lead crisis management, did not have formal space for the participation of sub-national governments. The federal government took unilateral decisions on every aspect of containing COVID and circulated those decisions downward. In most of the cases, the coordination was at the bureaucratic level. The federal government did not realize that the province and local governments were two years younger than the 2015 Constitution and they require constructive support in developing institutional capacity.
One important exogenous factor to reveal here was the protracted political in-fighting in the ruling party. Unrelated but concurrently with the upward surge in virus spread, the internal conflict in the ruling party was triumphing. It distracted the focus of political leaders including the Cabinet members for managing party conflict, thereby plummeting attention on COVID management (Shakya, 2020; Acharya & Thapa, 2021). Such political maneuvering led to a critical deficit in providing effective leadership by the federal government to the sub-national governments. The federal government faced instability, the parliament was dissolved repeatedly while the Supreme Court had to step in to defy the parliament dissolution and the provincial governments also saw the impact of national political maneuvering. The political tug-of-war impeded the coordinated functioning of the government as the top leadership had a priority on reformation of the government than managing the health crisis (Pandey, 2021). Amidst the pandemic mayhem, the factions of the ruling party organized several mass-gathering for influencing the other factions of the party. Such gatherings undermined the health safety measures- further increasing the risk of virus spread. The completely overlooked aspect was the engagement of leaders, who were also holding the executive responsibility, in pleasing their cadres, leaving executive priority almost suspended. At the time when the country needed national unity, and friendly dialogue among political actors and other stakeholders, the collaborative culture was almost non-existence.
Considering the externality of the pandemic, a few local governments spontaneously attempted horizontal partnerships in preparing quarantine centers, enhancing testing facilities, providing relief and medical care, and ensuring safety in public mobility. However, these initiatives were not systematic and not guided by a policy framework.
Coordination meeting
In round 2, the survey captured the number of meetings that local governments conducted with the federal government, provincial government, district administration office, and ward offices on the issues to combat COVID. Frequent meetings were conducted with the ward offices within the jurisdiction of local governments (88.8% said to have 1 to 5 meetings), followed by the district administration office (82.2% said to have 1 to 5 meetings), a federal government’s local agency.
On the contrary, the proportion of local governments reporting not having any meeting with the federal government was 57% and with the provincial government, it was 60%.
Table 4. Frequency of Coordination Meeting
R2= Second round of survey between October-November 2020 (sample 115). This question was not asked in round 2.
R3= Third round of survey between April-May 2021 (sample 753)
In addition, 35% of local governments in round 2 expressed some sort of disagreement in the ways that the federal government took decisions to deal with COVID, particularly in the issues of financing, lockdown, testing, tracing, quarantine, distribution of relief, and vaccines. The proportion of local governments reporting disagreement with the provincial government was slightly less than 30%. These disagreements were mainly in the way the federal government made decisions, the federal policies on lockdown, disproportionate sharing of financial resources (Bhandari, et al., 2020), medical support, distribution of medical supplies and vaccines, and deployment of health professionals. Sub-national governments have mainly criticized the tendency of unilateral decisions of the federal government to ignore the local context and requirements (Mainali, Tosun, & Yilmaz, 2021; Ghimire, 2021). The major deficit in pandemic control was the absence of the federal pandemic act. The CO VID response has been guided by the Infectious Disease Act 1964, the act which was functional in the erstwhile unitary system has been unresponsive to the federal structure. The Act does not recognize the roles of provincial and local governments but mandates agencies of the central government to exercise authority. Although the federal government introduced the COVID control ordinance in 2021, it failed to receive parliamentary approval, pushing COVID control back to half a century-old legislature, and causing lapses in intergovernmental relations.
On the other side, the inept functioning of provincial and local governments was equally responsible for ineffective vertical and horizontal coordination. Despite having low capacity, the local governments, as the first responder, played a relatively better role to contain the health crisis. The provincial governments, the medium order government having responsibility for providing leadership to local governments within their jurisdictions and negotiating with the federal government for effective delivery and leveraging backstopping for local governments and also having ownership of medium order hospitals, were largely criticized for their ineffective roles.
As Nepal's federal system is in its infancy, the structural arrangements to promote intergovernmental relations are yet to be institutionalized. Some coordination mechanisms such as the Inter-Provincial Council, National Coordination Councils, and other structures of coordination are provisioned in the Constitution and subsequent legislations, nonetheless, they are largely dysfunctional (Pokharel & Sapkota, 2021). The CCMC, a top-notch body to lead crisis management, did not have formal space for the participation of sub-national governments. The federal government took unilateral decisions on every aspect of containing COVID and circulated those decisions downward. In most of the cases, the coordination was at the bureaucratic level. The federal government did not realize that the province and local governments were two years younger than the 2015 Constitution and they require constructive support in developing institutional capacity.
One important exogenous factor to reveal here was the protracted political in-fighting in the ruling party. Unrelated but concurrently with the upward surge in virus spread, the internal conflict in the ruling party was triumphing. It distracted the focus of political leaders including the Cabinet members for managing party conflict, thereby plummeting attention on COVID management (Shakya, 2020; Acharya & Thapa, 2021). Such political maneuvering led to a critical deficit in providing effective leadership by the federal government to the sub-national governments. The federal government faced instability, the parliament was dissolved repeatedly while the Supreme Court had to step in to defy the parliament dissolution and the provincial governments also saw the impact of national political maneuvering. The political tug-of-war impeded the coordinated functioning of the government as the top leadership had a priority on reformation of the government than managing the health crisis (Pandey, 2021). Amidst the pandemic mayhem, the factions of the ruling party organized several mass-gathering for influencing the other factions of the party. Such gatherings undermined the health safety measures- further increasing the risk of virus spread. The completely overlooked aspect was the engagement of leaders, who were also holding the executive responsibility, in pleasing their cadres, leaving executive priority almost suspended. At the time when the country needed national unity, and friendly dialogue among political actors and other stakeholders, the collaborative culture was almost non-existence.
Considering the externality of the pandemic, a few local governments spontaneously attempted horizontal partnerships in preparing quarantine centers, enhancing testing facilities, providing relief and medical care, and ensuring safety in public mobility. However, these initiatives were not systematic and not guided by a policy framework.
Coordination meeting
In round 2, the survey captured the number of meetings that local governments conducted with the federal government, provincial government, district administration office, and ward offices on the issues to combat COVID. Frequent meetings were conducted with the ward offices within the jurisdiction of local governments (88.8% said to have 1 to 5 meetings), followed by the district administration office (82.2% said to have 1 to 5 meetings), a federal government’s local agency.
On the contrary, the proportion of local governments reporting not having any meeting with the federal government was 57% and with the provincial government, it was 60%.
Table 4. Frequency of Coordination Meeting
Frequency of meeting |
FG |
PG |
DAO |
WO |
None |
57.0 |
59.8 |
12.2 |
3.4 |
1 to 5 |
30.2 |
35.6 |
82.2 |
88.8 |
6 and more |
12.8 |
4.6 |
5.6 |
7.9 |
Total |
100.0 |
100.0 |
100.0 |
100.0 |
R2= Second round of survey between October-November 2020 (sample 115)
FG= Federal Government, PG= Provincial government, DAO= District Administration Office,
WO=Ward Office
Although the survey did not capture what mechanisms of coordination meetings the local governments attended with federal and provincial governments, it is apparent that most of the meetings might have been based on individual relations or bureaucratic formal processes. As discussed in an earlier section, there was no such functional formal structural arrangement in the federal government to allow provincial and local governments to participate in national coordination meetings. Coordination mechanisms that are in place, were largely dysfunctional. The district administration offices, which are the federal government's delegated office, have received a number of responsibilities in pandemic control. The district administration offices have been federally entrusted with functional and authoritative organizations having a long authority-exercising legacy (Pokharel, 2021). The federal government, through the pandemic act and other legislations, provides the district administration offices with both coordination and coercion authorities including exercising legal powers, mobilizing security forces and enforcing law and order, reducing the role of provincial and local governments (Institute for Integrated Development Studies [IIDS] & Nepal Institute for Policy Research [NIPoRe], 2021). This might have a positive response in coordination meetings between district administration offices and local governments, while such functional coordination mechanisms at the political level with federal and provincial governments do not exist.
The absence of such coordination mechanisms has limited the opportunities to build a strong intergovernmental relationship for managing the COVID crisis more competently and effectively. The local governments were in demand of technical, financial, and administrative support. The associations of local governments, the Municipal Association of Nepal for urban municipalities, and the National Association of Rural Municipalities for rural municipalities, could not provide effective leadership on behalf of the local governments to negotiate with provincial and federal governments. They organized a few experience-sharing meetings among the local governments and published a few newsletters and shared information. Their role was expected to have a larger scope to provide overall leadership and echo the concerns of local governments. It would then encourage the federal and provincial governments to address the concerns of local governments.
5. Discussion
As the first case of the virus was detected in early 2020, Nepal did not have single testing facilities. The samples were sent abroad for testing. In a short period, the testing facilities were expanded to over 100, of which nearly half are private testing centers. As the cases were growing, 36 dedicated hospitals were assigned for providing treatment to COVID patients, which as of now provide free treatment to the infected. The government made efforts to educate the public through the massive use of public media. There was widespread chaos and stereotyping in the early days of the pandemic. The patients were disgraced by both public and health professionals. Health workers also faced stigmatization. Nevertheless, the continuous public communication and the spread of the virus gradually corrected the publicly held opinion itself. For a health system that is asymmetrically distributed across the country, exacerbated by fricking pre-existing strengths, providing an equitable service has always been a challenge. The pandemic further exposed the inequity.
Nepal has been undergoing an unprecedented political and administrative transformation as enshrined by the 2015 Constitution. The main objective of the constitution is to safeguard the fundamental rights of the people by taking the country towards overall socio-economic development and establishing democratic governance at all levels. The federalist constitution has allocated the competences among the federal units where health crisis management is a shared function. As Nepal is in the process of implementing the constitutional architecture of state structure by devolving the functions and functionaries to the sub-national levels, the COVID crisis appeared as a litmus test for health governance.
Amidst the brawls of gaining clarity in appreciating the new governance structure and developing congruent infrastructures, the management of the pandemic provided an opportunity to examine the strengths and weaknesses of health governance. For a country with poor economic and governance infrastructure, dealing with a crisis of this scale required innovative and concerted efforts among the actors. The crisis that completely quivered even the well-institutionalized health governance systems (Freed, Kwon, Hannah, Gottlieb, & Roth, 2020; Dentico, 2021), Nepal’s experience is full of lessons and tragedies.
COVID has been a wake-up call for countries to assess their crisis management strategies and apply appropriate measures to strengthen health governance to cope with the pandemic. There could be different strategies to survive the crisis and protect the lives of people including minimizing harm to the economy and society. Studies around the globe have shown that concerted efforts of all the agencies responsible for managing crises are a must (Paquet & Schertzer, 2020; Schnabel & Hegele, 2021). In a country having better coordination and support system among the orders of the governments, managing the crisis was relatively better, or otherwise (Jüptner & Klimovský, 2021).
This paper argues that effective governance matters. More than that, leadership awareness and commitment matter. COVID was not like the 2015 earthquake that Nepal survived, where global support was overwhelmed. However, for COVID, countries were required to contest on their own, as it was a global pandemic, quivering everywhere. In such a situation, the competence of national leadership matters. Handling COVID is, therefore, a function of adaptive leadership competency, the capacity of health governance, resources mobilization, the existence of crisis management strategy, and the ability to marshal the agencies.
This paper, based on a survey, elucidates the perspectives of the relationships among the orders of the government, as perceived by the local governments. We see, in summary, a gross mismatch between federal arguments of effective coordination versus survey findings of persistent gaps in the government’s approach to handling the pandemic. The federal government made unilateral decisions in enforcing policies and guidelines and held provincial and local governments responsible for implementation without addressing their concerns. Other than the federal government’s initiative to form a high-level coordination committee, functional coordination was absent, leaving the sub-national governments functioning on their own. The pandemic was expected to narrow the distance between the federal units, unwantedly it further exacerbated the relationship (Gill & Sapkota, 2020). Intergovernmental dialogues did not take place as they were supposed to. Neither the federal government took the initiative, nor did the sub-national governments push for such dialogues. It left the activities of different agencies discrete, uncoordinated, and overlapped.
Local governments were engaged in social activities of prevention, as they were designated to do so, than in curative services. In the absence of clear division and understanding of roles and responsibilities, local governments have temptations to do higher-order activities such as management of hospitals, purchase of vaccines, enforcing lockdowns, and deployment of health professionals. The roles of local governments as the first responder to public concerns should be valued positively. They used their limited strengths to provide preventive services, provide leadership to people, and facilitate the service process. However, most of their efforts were intuitive. For example, the unplanned construction of sub-standard quarantine centers by local governments was criticized for misuse of public resources.
The effect of delays in the completion of the transition was exhibited during the pandemic. The federal government was supposed to hand over the centrally owned infrastructures in the erstwhile system to provincial and local governments in the inspirit of the 2015 Constitution. Protracting delays in transfers of functions and functionaries made the sub-national governments deficient in facilities that are related to health services. The local governments stated that lack of health facilities, resources, and coordination as the major challenges to managing COVID. Important to note is, that these challenges are not the ones that appeared during COVID but are enduring disorders of health governance in Nepal. However, the government took some immediate initiatives to expand health facilities amidst the pandemic. Its impacts have been observed in the subsequent rounds of surveys, the local governments reported the said challenges declined considerably over the periods.
Survey results show declining intergovernmental support and coordination as the pandemic prolonged. Such discontinuation could be because of the absence of a prospective plan for coordination. In the beginning, the authorities, particularly the political leadership, took COVID as an opportunity to glorify. For example, when there was the first case, the Chief Minister of Gandaki Province made an individual inquiry to the patient, visited the hospitals, instructed the hospital, and made other interactions. It drew media attention. Later, as the cases were rising no such visit or response was noticed. In addition, the government-owned insurance board introduced a COVID insurance scheme to provide a cash payment to COVID infected. The scheme was considered a cherished initiative of the government. But as the cases overwhelmed, the government was forced to terminate the scheme, leaving the claims of hundreds of thousands of eligible insurers unsettled. Government still has to bail out over 10 billion Nepali rupees to the insurance board, a hyped initiative that eventually turned into a burden. It indicates the misalignment of government priority.
Nevertheless, Nepal’s efforts to contain viruses have to be evaluated in both prospects- the strengths and weaknesses. For a country with a crippling economy and transitioning governance, dealing with a pandemic of such an immense scale has been full of challenges. Three years after the pandemic, the world has made significant progress in combating the virus, yet advanced economies are struggling to eliminate the pandemic. In Nepal, the frontline health workers stood as the shield while the security forces took the burdens of backstopping. While the district administration offices, an extension of the federal government, were responsible for maintaining law, order, and coordination at the local level, the local governments responded to public grievances, condensing the public frustration with federal and provincial governments. What Nepal was missing was proactive, rational, and effective political leadership, particularly at the federal and provincial levels. It led to a disdain for an intergovernmental relationship (Nepal Health Research Council [NHRC], 2020; Rayamajhee, et al., 2021), rambling opportunities to institutionalize functional coordination mechanisms.
In the mayhem pandemic aftermath, a reflective analysis of Nepal’s efforts for COVID management has several stories to share with the global audience. Nepal has survived several crises- both natural and anthropogenic and will continue to face them as it is in the higher-order risk zone of different types of disasters. While COVID is considered partly anthropogenic (Deakin & Meng, 2020), human activities have been both the causes for exacerbation and remedy. In such cases, the effective leadership of the government becomes apparent to survive the crisis. The inept functioning of the government and its inability to mobilize the networks in a concerted way may cost dearer, particularly in the time of crisis. Nepal’s case is useful for any polity with a similar socio-economic structure and particularly may be referenced to the country that is experimenting with a federal form of decentralized governance.
6. Conclusion
Surviving the crises like COVID pandemic shall be a collaborative effort among the governing agencies. Public health is a shared responsibility among the tiers of government, and a deliberate mechanism of coordination should be in place. Nepal has recently embarked on a federalized system of governance that transformed the state structure into a more decentralized form of governance. Amidst the progression of transition, managing the COVID crisis has been a real test for assessing the challenges in the crisis management system and devising interventions to improve it further.
For surviving crises in the future, the following three lessons are derived from this paper:
Strengthening sub-national health governance: Sub-national governments have asserted reduced roles over the rounds of survey, owing to unclear framework and allocation of responsibilities. Strengthening sub-national governments would reduce the burden on the federal government and would produce a healthier impact on overall crisis management.
Strengthen linkages and rheostat exogenous influence: Ineffective interlinkages among the orders of government could be due to exogenous factors (political rift within the ruling party[1], undesired political activities, the residual impact of the erstwhile system, political transition), and systemic factors (lack of clear framework, leadership practices, crisis management capacity, health service capacity). It is necessary to avoid exogenous factors and institutionalize a systemic framework of cooperation.
Missing links to managing links: Sub-national governments should be recognized as part of the whole of government. Subnational governments could be mobilized better by providing a clear framework and leadership to transform 'missing link' into 'managing link'.
FG= Federal Government, PG= Provincial government, DAO= District Administration Office,
WO=Ward Office
Although the survey did not capture what mechanisms of coordination meetings the local governments attended with federal and provincial governments, it is apparent that most of the meetings might have been based on individual relations or bureaucratic formal processes. As discussed in an earlier section, there was no such functional formal structural arrangement in the federal government to allow provincial and local governments to participate in national coordination meetings. Coordination mechanisms that are in place, were largely dysfunctional. The district administration offices, which are the federal government's delegated office, have received a number of responsibilities in pandemic control. The district administration offices have been federally entrusted with functional and authoritative organizations having a long authority-exercising legacy (Pokharel, 2021). The federal government, through the pandemic act and other legislations, provides the district administration offices with both coordination and coercion authorities including exercising legal powers, mobilizing security forces and enforcing law and order, reducing the role of provincial and local governments (Institute for Integrated Development Studies [IIDS] & Nepal Institute for Policy Research [NIPoRe], 2021). This might have a positive response in coordination meetings between district administration offices and local governments, while such functional coordination mechanisms at the political level with federal and provincial governments do not exist.
The absence of such coordination mechanisms has limited the opportunities to build a strong intergovernmental relationship for managing the COVID crisis more competently and effectively. The local governments were in demand of technical, financial, and administrative support. The associations of local governments, the Municipal Association of Nepal for urban municipalities, and the National Association of Rural Municipalities for rural municipalities, could not provide effective leadership on behalf of the local governments to negotiate with provincial and federal governments. They organized a few experience-sharing meetings among the local governments and published a few newsletters and shared information. Their role was expected to have a larger scope to provide overall leadership and echo the concerns of local governments. It would then encourage the federal and provincial governments to address the concerns of local governments.
5. Discussion
As the first case of the virus was detected in early 2020, Nepal did not have single testing facilities. The samples were sent abroad for testing. In a short period, the testing facilities were expanded to over 100, of which nearly half are private testing centers. As the cases were growing, 36 dedicated hospitals were assigned for providing treatment to COVID patients, which as of now provide free treatment to the infected. The government made efforts to educate the public through the massive use of public media. There was widespread chaos and stereotyping in the early days of the pandemic. The patients were disgraced by both public and health professionals. Health workers also faced stigmatization. Nevertheless, the continuous public communication and the spread of the virus gradually corrected the publicly held opinion itself. For a health system that is asymmetrically distributed across the country, exacerbated by fricking pre-existing strengths, providing an equitable service has always been a challenge. The pandemic further exposed the inequity.
Nepal has been undergoing an unprecedented political and administrative transformation as enshrined by the 2015 Constitution. The main objective of the constitution is to safeguard the fundamental rights of the people by taking the country towards overall socio-economic development and establishing democratic governance at all levels. The federalist constitution has allocated the competences among the federal units where health crisis management is a shared function. As Nepal is in the process of implementing the constitutional architecture of state structure by devolving the functions and functionaries to the sub-national levels, the COVID crisis appeared as a litmus test for health governance.
Amidst the brawls of gaining clarity in appreciating the new governance structure and developing congruent infrastructures, the management of the pandemic provided an opportunity to examine the strengths and weaknesses of health governance. For a country with poor economic and governance infrastructure, dealing with a crisis of this scale required innovative and concerted efforts among the actors. The crisis that completely quivered even the well-institutionalized health governance systems (Freed, Kwon, Hannah, Gottlieb, & Roth, 2020; Dentico, 2021), Nepal’s experience is full of lessons and tragedies.
COVID has been a wake-up call for countries to assess their crisis management strategies and apply appropriate measures to strengthen health governance to cope with the pandemic. There could be different strategies to survive the crisis and protect the lives of people including minimizing harm to the economy and society. Studies around the globe have shown that concerted efforts of all the agencies responsible for managing crises are a must (Paquet & Schertzer, 2020; Schnabel & Hegele, 2021). In a country having better coordination and support system among the orders of the governments, managing the crisis was relatively better, or otherwise (Jüptner & Klimovský, 2021).
This paper argues that effective governance matters. More than that, leadership awareness and commitment matter. COVID was not like the 2015 earthquake that Nepal survived, where global support was overwhelmed. However, for COVID, countries were required to contest on their own, as it was a global pandemic, quivering everywhere. In such a situation, the competence of national leadership matters. Handling COVID is, therefore, a function of adaptive leadership competency, the capacity of health governance, resources mobilization, the existence of crisis management strategy, and the ability to marshal the agencies.
This paper, based on a survey, elucidates the perspectives of the relationships among the orders of the government, as perceived by the local governments. We see, in summary, a gross mismatch between federal arguments of effective coordination versus survey findings of persistent gaps in the government’s approach to handling the pandemic. The federal government made unilateral decisions in enforcing policies and guidelines and held provincial and local governments responsible for implementation without addressing their concerns. Other than the federal government’s initiative to form a high-level coordination committee, functional coordination was absent, leaving the sub-national governments functioning on their own. The pandemic was expected to narrow the distance between the federal units, unwantedly it further exacerbated the relationship (Gill & Sapkota, 2020). Intergovernmental dialogues did not take place as they were supposed to. Neither the federal government took the initiative, nor did the sub-national governments push for such dialogues. It left the activities of different agencies discrete, uncoordinated, and overlapped.
Local governments were engaged in social activities of prevention, as they were designated to do so, than in curative services. In the absence of clear division and understanding of roles and responsibilities, local governments have temptations to do higher-order activities such as management of hospitals, purchase of vaccines, enforcing lockdowns, and deployment of health professionals. The roles of local governments as the first responder to public concerns should be valued positively. They used their limited strengths to provide preventive services, provide leadership to people, and facilitate the service process. However, most of their efforts were intuitive. For example, the unplanned construction of sub-standard quarantine centers by local governments was criticized for misuse of public resources.
The effect of delays in the completion of the transition was exhibited during the pandemic. The federal government was supposed to hand over the centrally owned infrastructures in the erstwhile system to provincial and local governments in the inspirit of the 2015 Constitution. Protracting delays in transfers of functions and functionaries made the sub-national governments deficient in facilities that are related to health services. The local governments stated that lack of health facilities, resources, and coordination as the major challenges to managing COVID. Important to note is, that these challenges are not the ones that appeared during COVID but are enduring disorders of health governance in Nepal. However, the government took some immediate initiatives to expand health facilities amidst the pandemic. Its impacts have been observed in the subsequent rounds of surveys, the local governments reported the said challenges declined considerably over the periods.
Survey results show declining intergovernmental support and coordination as the pandemic prolonged. Such discontinuation could be because of the absence of a prospective plan for coordination. In the beginning, the authorities, particularly the political leadership, took COVID as an opportunity to glorify. For example, when there was the first case, the Chief Minister of Gandaki Province made an individual inquiry to the patient, visited the hospitals, instructed the hospital, and made other interactions. It drew media attention. Later, as the cases were rising no such visit or response was noticed. In addition, the government-owned insurance board introduced a COVID insurance scheme to provide a cash payment to COVID infected. The scheme was considered a cherished initiative of the government. But as the cases overwhelmed, the government was forced to terminate the scheme, leaving the claims of hundreds of thousands of eligible insurers unsettled. Government still has to bail out over 10 billion Nepali rupees to the insurance board, a hyped initiative that eventually turned into a burden. It indicates the misalignment of government priority.
Nevertheless, Nepal’s efforts to contain viruses have to be evaluated in both prospects- the strengths and weaknesses. For a country with a crippling economy and transitioning governance, dealing with a pandemic of such an immense scale has been full of challenges. Three years after the pandemic, the world has made significant progress in combating the virus, yet advanced economies are struggling to eliminate the pandemic. In Nepal, the frontline health workers stood as the shield while the security forces took the burdens of backstopping. While the district administration offices, an extension of the federal government, were responsible for maintaining law, order, and coordination at the local level, the local governments responded to public grievances, condensing the public frustration with federal and provincial governments. What Nepal was missing was proactive, rational, and effective political leadership, particularly at the federal and provincial levels. It led to a disdain for an intergovernmental relationship (Nepal Health Research Council [NHRC], 2020; Rayamajhee, et al., 2021), rambling opportunities to institutionalize functional coordination mechanisms.
In the mayhem pandemic aftermath, a reflective analysis of Nepal’s efforts for COVID management has several stories to share with the global audience. Nepal has survived several crises- both natural and anthropogenic and will continue to face them as it is in the higher-order risk zone of different types of disasters. While COVID is considered partly anthropogenic (Deakin & Meng, 2020), human activities have been both the causes for exacerbation and remedy. In such cases, the effective leadership of the government becomes apparent to survive the crisis. The inept functioning of the government and its inability to mobilize the networks in a concerted way may cost dearer, particularly in the time of crisis. Nepal’s case is useful for any polity with a similar socio-economic structure and particularly may be referenced to the country that is experimenting with a federal form of decentralized governance.
6. Conclusion
Surviving the crises like COVID pandemic shall be a collaborative effort among the governing agencies. Public health is a shared responsibility among the tiers of government, and a deliberate mechanism of coordination should be in place. Nepal has recently embarked on a federalized system of governance that transformed the state structure into a more decentralized form of governance. Amidst the progression of transition, managing the COVID crisis has been a real test for assessing the challenges in the crisis management system and devising interventions to improve it further.
For surviving crises in the future, the following three lessons are derived from this paper:
Strengthening sub-national health governance: Sub-national governments have asserted reduced roles over the rounds of survey, owing to unclear framework and allocation of responsibilities. Strengthening sub-national governments would reduce the burden on the federal government and would produce a healthier impact on overall crisis management.
Strengthen linkages and rheostat exogenous influence: Ineffective interlinkages among the orders of government could be due to exogenous factors (political rift within the ruling party[1], undesired political activities, the residual impact of the erstwhile system, political transition), and systemic factors (lack of clear framework, leadership practices, crisis management capacity, health service capacity). It is necessary to avoid exogenous factors and institutionalize a systemic framework of cooperation.
Missing links to managing links: Sub-national governments should be recognized as part of the whole of government. Subnational governments could be mobilized better by providing a clear framework and leadership to transform 'missing link' into 'managing link'.
References
Acharya, K. K. (2018). The capacity of local governments in Nepal: From government to governance and governability?Asia Pacific Journal of Public Administration, 40(3), 186-197. doi:https://doi.org/10.1080/23276665.2018.1525842
Acharya, M. R., Upadhyay, P., & Acharya, A. (2020). Assignment of functions across levels of government in Nepal.Kathmandu: The Asia Foundation & Australian Aid.
Acharya, Y. R., & Thapa, P. B. (2021, June 29). Nepal's Democracy in Peril. Retrieved July 14, 2022, from International Republican Institute: https://www.iri.org/news/nepals-democracy-in-peril/
Bagale, S. (2020, September 20). CCMC Becomes Almost Obsolete. Retrieved June 22, 2022, from Setopati: https://en.setopati.com/political/153956
Bell, J. A., & Nuzzo, J. B. (2021). Global health security index: Advancing collective action and accountability amidglobal crisis. Washington DC: Nuclear Threat Initiative.
Bhandari, C., Bhurtel, A., Callen, M., Kayastha, C., Lama, T., Pande, R., . . . Wolf, A. (2020). COVID-19 and Nepal's health financing: Insights and recommendations based on local government response during full lockdown. Yale: Yale Economic Growth Center, Governance Lab, Nepal Administrative Staff College, The London School of Economics and Political Science.
Bhandari, G. P., Dixit, S. M., Ghimire, U., & Maskey, M. K. (2010). Outbreak investigation of diarrheal diseases in Jajarkot. Journal of Nepal Health Research Council, 7(2), 66-68. Central Bureau of Statistics. (2022). National Population Census 2021: Preliminary Report (in Nepali). Kathmandu: Central Bureau of Statistics.
Deakin, S., & Meng, G. (2020). The governance of Covid-19: Anthropogenic risk, evolutionary learning, and the future of the social state. Industrial Law Journal, 49(4), 539-594. doi:https://doi.org/10.1093/indlaw/dwaa027
Democracy Resource Center Nepal. (2020). Role of local governments in COVID-19 prevention and quarantinemanagement. Kathmandu: Democracy Resource Center Nepal. Dentico, N. (2021). The breathing catastrophe: COVID-19 and global health governance. Development, 64, 4-12. doi:https://doi.org/10.1057/s41301-021-00296-y
Dhungana, H., Pokharel, T., & Poudel, A. (2021). Federal governance system of Nepal: A synopsis. Lalitpur: Centre for Federalism Studies at NASC & The Asia Foundation.
Freed, J. S., Kwon, S. Y., Hannah, J. E., Gottlieb, M., & Roth, R. (2020). Which country is truly developed? COVID-19 has answered the question. Annals of Global Health, 86(1), 51. doi: 10.5334/aogh.2894
Ghimire, J. (2021). How Nepal has responded COVID-19 in first and second wave: Reactive or prepared? MOJ Public Health, 10(3), 56-57. doi:https://doi.org/10.15406/mojph.2021.10.00361
Ghimire, R. (2021, May 20). Poor coordination among 3 tiers of government mars Nepal COVID-19 response. https://english.onlinekhabar.com/poor-coordination-among-3-tiers-of-government-mars-nepal-covid-19-response.html
Gill, P., & Sapkota, J. R. (2020, June 29). COVID-19: Nepal in crisis. https://thediplomat.com/2020/06/covid-19-nepal-in-crisis/
Institute for Integrated Development Studies [IIDS] & Nepal Institute for Policy Research [NIPoRe]. (2021). Nepal risk outlook. Kathmandu: Institute for Integrated Development Studies [IIDS] & Nepal Institute for Policy Research [NIPoRe].
Jüptner, P., & Klimovský, D. (2021). Vertical and horizontal intergovernmental relations during the first wave of the COVID-19 crisis: Experience from the extremely fragmented CEE countries. Local Government Studies, 1-19. doi:https://doi.org/10.1080/03003930.2021.1944858
Mainali, R., Tosun, M. S., & Yilmaz, S. (2021). Local response to the COVID‐19 pandemic: The case of Nepal. Public Administration and Development, 41(3), 128-134. doi:https://dx.doi.org/10.1002%2Fpad.1953
McEwen, N., Petersohn, B., & Swan, C. B. (2015). Intergovernmental relations and parliamentary scrutiny: A comparative overview. London: The University of Edinburgh, Centre on Constitutional Change & Swansea University.
Ministry of Finance [MoF]. (2022). Budget Speech (English). https://mof.gov.np/site/publication-category/87
Ministry of Finance. (2021). Annual Budget Book. Kathmandu: Ministry of Finance.
Ministry of Health and Population [MoHP]. (2018). Number of Health Facilities in Nepal. https://heoc.mohp.gov.np/service/number-of-health-facilities-in-nepal/
Ministry of Health and Population [MoHP]. (2019). National Health Policy 2019. Kathmandu: Ministry of Health and Population.
Ministry of Home Affairs [MoHA]. (2017). Nepal Disaster Report 2017: The Road to Sendai. Kathmandu: Ministry of Home Affairs.
Morphet, J. (2008). Modern local government. London: SAGE Publications Ltd.
National Planning Commission [NPC]. (2015). Nepal earthquake 2015: Post-disaster needs assessment. Kathmandu: NPC.
Nepal Health Research Council [NHRC]. (2020). Assessment of compliance with SMS measures against COVID-19 in Kathmandu Valley. Kathmandu: Nepal Health Research Council [NHRC].
Nepal Health Research Council [NHRC]. (2020). Rapid assessment of COVID-19 related policy audit in Nepal.Kathmandu: Nepal Health Research Council.
Pandey, L. (2021, May 13). Nepal: Political Tug-of-War Hampers Efforts to Tackle COVID. https://www.dw.com/en/nepal-political-tug-of-war-hampers-efforts-to-tackle-covid/a-57520469
Paquet, M., & Schertzer, R. (2020). COVID-19 as a complex intergovernmental problem. Canadian Journal of Political Science, 53, 343–347. doi:https://doi.org/10.1017/S0008423920000281
Phillimore, J. (2013). Understanding intergovernmental relations: Key features and trends. Australian Journal of Public Administration, 72(3), 228-238. doi:0.1111/1467-8500.12025
Poirier, J., & Saunders, C. (2010). Cooperative mechanisms and intergovernmental relations in federal regimes. In R. Chattopadhyay, & K. Nerenberg (Eds.), Intergovernmental Relations in Federal Systems (pp. 3-8). Ontario: Forum of Federations.
Pokharel, G. (2021, September 24). Nepal federalism has made CDOs, once the kings of districts, lose powers and relevance. https://english.onlinekhabar.com/cdo-nepal-responsibilities.html
Pokharel, T., & Dahal, A. (2020). 2015 Gorkha Earthquake, New Constitution and Local Resilience in Nepal. In N. Akira, & K. Masao (Eds.), Local Governance in the Age of Technological Transformation and Global Uncertainty (pp. 49-74). Tokyo: EROPA Local Government Center. ps://www.soumu.go.jp/main_content/000695477.pdf
Pokharel, T., & Sapkota, L. N. (2021). Intergovernmental fiscal relations in Nepal: Unfolding dynamics and dimensions.Kathmandu: Centre for Federalism Studies at NASC and The Asia Foundation.
Pradhan, T. R., & Prasain, S. (2021, September 18). Big confusion as top body responding to COVID-19 becomes defunct.https://kathmandupost.com/national/2021/09/18/big-confusion-as-top-body-responding-to-covid-19-becomes-defunct
Rayamajhee, B., Pokhrel, A., Syangtan, G., Khadka, S., Lama, B., Rawal, L. B., . . . Yadav, U. N. (2021). How well the government of Nepal is responding to COVID-19? An experience from a resource-limited country to confront unprecedented pandemic. Frontiers in Public Health. doi:https://doi.org/10.3389/fpubh.2021.597808
Sah, P., Mandal, A. K., Saud, B., Yadav, S. K., Sah, S. K., Gyawali, M., & Karn, S. K. (2022). Knowledge, practices and compliance related to COVID-19 among Nepalese population in Province 2, Nepal. Dialogues in Health, 1. doi:https://doi.org/10.1016/j.dialog.2022.100002
Schnabel, J., & Hegele, Y. (2021). Explaining intergovernmental coordination during the COVID-19 pandemic: Responses in Australia, Canada, Germany, and Switzerland. Publius, 537-569. doi:https://doi.org/10.1093/publius/pjab011
Shakya, S. (2020, June 11). Political manoeuvres compromise Nepal’s COVID-19 response. Retrieved July 13, 2022, from East Asian Forum: https://www.eastasiaforum.org/2020/06/11/political-manoeuvres-compromise-nepals-covid-19-response/
Silva, C. N. (2022). Local government and the COVID-19 Pandemic: An introduction. In C. N. Silva (Ed.), Local Government and the COVID-19 Pandemic: A Global Perspective (p. 1026). London: Springer Nature.
Singh, R., & Subedi, M. (2020). COVID-19 and stigma: Social discrimination towards frontline healthcare providers and COVID-19 recovered patients in Nepal. Asian Journal of Psychiatry, 53, 1-2. doi:10.1016/j.ajp.2020.102222
Thapa, R., Bam, K., Tiwari, P., Sinha, T. K., & Dahal, S. (2019). Implementing federalism in the health system of Nepal: Opportunities and challenges. International Journal of Health Policy and Management, 8(4), 195-198. doi:https://doi.org/10.15171/ijhpm.2018.121
The World Bank. (2022). Current health expenditure (% of GDP)- World, Nepal. https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS?end=2019&locations=1W-NP&start=2012&view=chart
World Life Expectancy. (2022, April 10). Health profile: Nepal. https://www.worldlifeexpectancy.com/country-health-profile/nepal
Acharya, K. K. (2018). The capacity of local governments in Nepal: From government to governance and governability?Asia Pacific Journal of Public Administration, 40(3), 186-197. doi:https://doi.org/10.1080/23276665.2018.1525842
Acharya, M. R., Upadhyay, P., & Acharya, A. (2020). Assignment of functions across levels of government in Nepal.Kathmandu: The Asia Foundation & Australian Aid.
Acharya, Y. R., & Thapa, P. B. (2021, June 29). Nepal's Democracy in Peril. Retrieved July 14, 2022, from International Republican Institute: https://www.iri.org/news/nepals-democracy-in-peril/
Bagale, S. (2020, September 20). CCMC Becomes Almost Obsolete. Retrieved June 22, 2022, from Setopati: https://en.setopati.com/political/153956
Bell, J. A., & Nuzzo, J. B. (2021). Global health security index: Advancing collective action and accountability amidglobal crisis. Washington DC: Nuclear Threat Initiative.
Bhandari, C., Bhurtel, A., Callen, M., Kayastha, C., Lama, T., Pande, R., . . . Wolf, A. (2020). COVID-19 and Nepal's health financing: Insights and recommendations based on local government response during full lockdown. Yale: Yale Economic Growth Center, Governance Lab, Nepal Administrative Staff College, The London School of Economics and Political Science.
Bhandari, G. P., Dixit, S. M., Ghimire, U., & Maskey, M. K. (2010). Outbreak investigation of diarrheal diseases in Jajarkot. Journal of Nepal Health Research Council, 7(2), 66-68. Central Bureau of Statistics. (2022). National Population Census 2021: Preliminary Report (in Nepali). Kathmandu: Central Bureau of Statistics.
Deakin, S., & Meng, G. (2020). The governance of Covid-19: Anthropogenic risk, evolutionary learning, and the future of the social state. Industrial Law Journal, 49(4), 539-594. doi:https://doi.org/10.1093/indlaw/dwaa027
Democracy Resource Center Nepal. (2020). Role of local governments in COVID-19 prevention and quarantinemanagement. Kathmandu: Democracy Resource Center Nepal. Dentico, N. (2021). The breathing catastrophe: COVID-19 and global health governance. Development, 64, 4-12. doi:https://doi.org/10.1057/s41301-021-00296-y
Dhungana, H., Pokharel, T., & Poudel, A. (2021). Federal governance system of Nepal: A synopsis. Lalitpur: Centre for Federalism Studies at NASC & The Asia Foundation.
Freed, J. S., Kwon, S. Y., Hannah, J. E., Gottlieb, M., & Roth, R. (2020). Which country is truly developed? COVID-19 has answered the question. Annals of Global Health, 86(1), 51. doi: 10.5334/aogh.2894
Ghimire, J. (2021). How Nepal has responded COVID-19 in first and second wave: Reactive or prepared? MOJ Public Health, 10(3), 56-57. doi:https://doi.org/10.15406/mojph.2021.10.00361
Ghimire, R. (2021, May 20). Poor coordination among 3 tiers of government mars Nepal COVID-19 response. https://english.onlinekhabar.com/poor-coordination-among-3-tiers-of-government-mars-nepal-covid-19-response.html
Gill, P., & Sapkota, J. R. (2020, June 29). COVID-19: Nepal in crisis. https://thediplomat.com/2020/06/covid-19-nepal-in-crisis/
Institute for Integrated Development Studies [IIDS] & Nepal Institute for Policy Research [NIPoRe]. (2021). Nepal risk outlook. Kathmandu: Institute for Integrated Development Studies [IIDS] & Nepal Institute for Policy Research [NIPoRe].
Jüptner, P., & Klimovský, D. (2021). Vertical and horizontal intergovernmental relations during the first wave of the COVID-19 crisis: Experience from the extremely fragmented CEE countries. Local Government Studies, 1-19. doi:https://doi.org/10.1080/03003930.2021.1944858
Mainali, R., Tosun, M. S., & Yilmaz, S. (2021). Local response to the COVID‐19 pandemic: The case of Nepal. Public Administration and Development, 41(3), 128-134. doi:https://dx.doi.org/10.1002%2Fpad.1953
McEwen, N., Petersohn, B., & Swan, C. B. (2015). Intergovernmental relations and parliamentary scrutiny: A comparative overview. London: The University of Edinburgh, Centre on Constitutional Change & Swansea University.
Ministry of Finance [MoF]. (2022). Budget Speech (English). https://mof.gov.np/site/publication-category/87
Ministry of Finance. (2021). Annual Budget Book. Kathmandu: Ministry of Finance.
Ministry of Health and Population [MoHP]. (2018). Number of Health Facilities in Nepal. https://heoc.mohp.gov.np/service/number-of-health-facilities-in-nepal/
Ministry of Health and Population [MoHP]. (2019). National Health Policy 2019. Kathmandu: Ministry of Health and Population.
Ministry of Home Affairs [MoHA]. (2017). Nepal Disaster Report 2017: The Road to Sendai. Kathmandu: Ministry of Home Affairs.
Morphet, J. (2008). Modern local government. London: SAGE Publications Ltd.
National Planning Commission [NPC]. (2015). Nepal earthquake 2015: Post-disaster needs assessment. Kathmandu: NPC.
Nepal Health Research Council [NHRC]. (2020). Assessment of compliance with SMS measures against COVID-19 in Kathmandu Valley. Kathmandu: Nepal Health Research Council [NHRC].
Nepal Health Research Council [NHRC]. (2020). Rapid assessment of COVID-19 related policy audit in Nepal.Kathmandu: Nepal Health Research Council.
Pandey, L. (2021, May 13). Nepal: Political Tug-of-War Hampers Efforts to Tackle COVID. https://www.dw.com/en/nepal-political-tug-of-war-hampers-efforts-to-tackle-covid/a-57520469
Paquet, M., & Schertzer, R. (2020). COVID-19 as a complex intergovernmental problem. Canadian Journal of Political Science, 53, 343–347. doi:https://doi.org/10.1017/S0008423920000281
Phillimore, J. (2013). Understanding intergovernmental relations: Key features and trends. Australian Journal of Public Administration, 72(3), 228-238. doi:0.1111/1467-8500.12025
Poirier, J., & Saunders, C. (2010). Cooperative mechanisms and intergovernmental relations in federal regimes. In R. Chattopadhyay, & K. Nerenberg (Eds.), Intergovernmental Relations in Federal Systems (pp. 3-8). Ontario: Forum of Federations.
Pokharel, G. (2021, September 24). Nepal federalism has made CDOs, once the kings of districts, lose powers and relevance. https://english.onlinekhabar.com/cdo-nepal-responsibilities.html
Pokharel, T., & Dahal, A. (2020). 2015 Gorkha Earthquake, New Constitution and Local Resilience in Nepal. In N. Akira, & K. Masao (Eds.), Local Governance in the Age of Technological Transformation and Global Uncertainty (pp. 49-74). Tokyo: EROPA Local Government Center. ps://www.soumu.go.jp/main_content/000695477.pdf
Pokharel, T., & Sapkota, L. N. (2021). Intergovernmental fiscal relations in Nepal: Unfolding dynamics and dimensions.Kathmandu: Centre for Federalism Studies at NASC and The Asia Foundation.
Pradhan, T. R., & Prasain, S. (2021, September 18). Big confusion as top body responding to COVID-19 becomes defunct.https://kathmandupost.com/national/2021/09/18/big-confusion-as-top-body-responding-to-covid-19-becomes-defunct
Rayamajhee, B., Pokhrel, A., Syangtan, G., Khadka, S., Lama, B., Rawal, L. B., . . . Yadav, U. N. (2021). How well the government of Nepal is responding to COVID-19? An experience from a resource-limited country to confront unprecedented pandemic. Frontiers in Public Health. doi:https://doi.org/10.3389/fpubh.2021.597808
Sah, P., Mandal, A. K., Saud, B., Yadav, S. K., Sah, S. K., Gyawali, M., & Karn, S. K. (2022). Knowledge, practices and compliance related to COVID-19 among Nepalese population in Province 2, Nepal. Dialogues in Health, 1. doi:https://doi.org/10.1016/j.dialog.2022.100002
Schnabel, J., & Hegele, Y. (2021). Explaining intergovernmental coordination during the COVID-19 pandemic: Responses in Australia, Canada, Germany, and Switzerland. Publius, 537-569. doi:https://doi.org/10.1093/publius/pjab011
Shakya, S. (2020, June 11). Political manoeuvres compromise Nepal’s COVID-19 response. Retrieved July 13, 2022, from East Asian Forum: https://www.eastasiaforum.org/2020/06/11/political-manoeuvres-compromise-nepals-covid-19-response/
Silva, C. N. (2022). Local government and the COVID-19 Pandemic: An introduction. In C. N. Silva (Ed.), Local Government and the COVID-19 Pandemic: A Global Perspective (p. 1026). London: Springer Nature.
Singh, R., & Subedi, M. (2020). COVID-19 and stigma: Social discrimination towards frontline healthcare providers and COVID-19 recovered patients in Nepal. Asian Journal of Psychiatry, 53, 1-2. doi:10.1016/j.ajp.2020.102222
Thapa, R., Bam, K., Tiwari, P., Sinha, T. K., & Dahal, S. (2019). Implementing federalism in the health system of Nepal: Opportunities and challenges. International Journal of Health Policy and Management, 8(4), 195-198. doi:https://doi.org/10.15171/ijhpm.2018.121
The World Bank. (2022). Current health expenditure (% of GDP)- World, Nepal. https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS?end=2019&locations=1W-NP&start=2012&view=chart
World Life Expectancy. (2022, April 10). Health profile: Nepal. https://www.worldlifeexpectancy.com/country-health-profile/nepal
Acknowledgements
The Author acknowledges Yale Economic Growth Center, London School of Economics and Political Sciences, Governance Lab Nepal, and Nepal Administrative Staff College for providing access to data on the Local and Provincial Government Survey.
The Author acknowledges Yale Economic Growth Center, London School of Economics and Political Sciences, Governance Lab Nepal, and Nepal Administrative Staff College for providing access to data on the Local and Provincial Government Survey.